Overview:
Rapid screening methods for heart failure (leading cause of unplanned hospitalizations and healthcare costs) in patients without symptoms are limited. This study validated PMcardio LVEF AI ECG model in identifying reduced heart function on widely accessible 12-lead ECGs. In a study of over 100-thousand patients, PMcardio demonstrated high performance (AUC 0.963) in detecting patients with reduced heart function offering a fast, non-invasive and scalable screening tool.
Published In: Circulation (AHA Journals) – presented at the American Heart Association (AHA) 2024 Scientific Sessions
Presented Date: November 11, 2024
Background
Though echocardiography is the cornerstone of cardiac function assessment in specialized practice, there is a lack of point-of-care tools for immediate evaluation of left ventricular ejection fraction (LVEF) in current practice facilitating the early identification of patients at risk for heart failure who may benefit from further echocardiographic evaluation.
We sought to develop and validate artificial intelligence (AI) models to identify reduced LVEF from a single 12-lead ECG using a smartphone application.
Methods
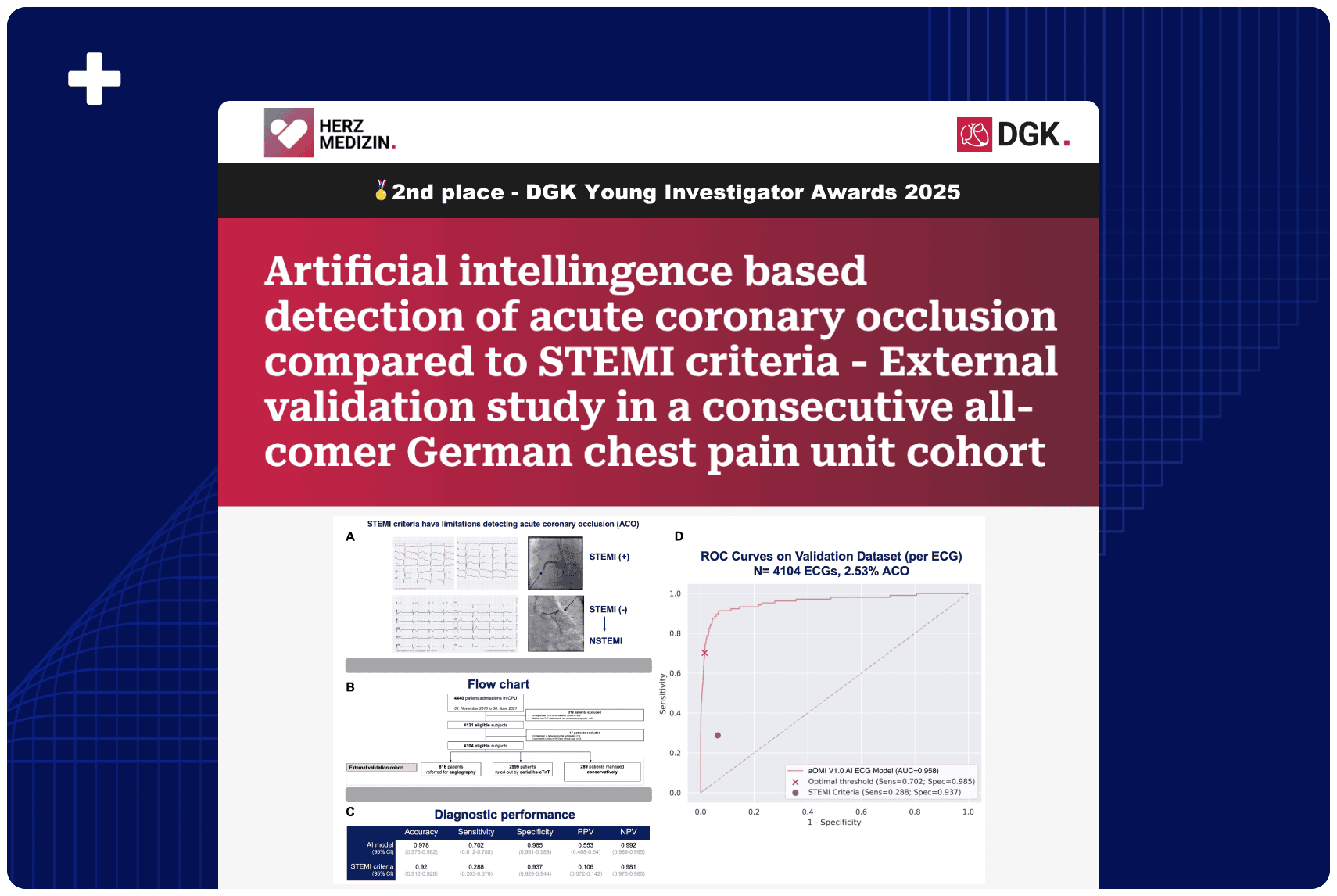
We sourced all ECGs and transthoracic echocardiograms (TTEs) recorded between 2011 and 2021. ECGs were paired with TTEs conducted within a 24-hour window and were randomly divided into the model development dataset (50%) and validation dataset (50%). Two AI-ECG models were created: one to detect LVEF ≤40% and another for LVEF <50%, following the AHA definition of heart failure. These models were coupled with smartphone-based ECG digitization technology. Performance metrics included area under the receiver operating characteristic curve (AUC), sensitivity, specificity, positive predictive value (PPV), negative predictive value (NPV), and F1-score.
Results
A total of 1,205,370 ECGs and 291,433 TTEs were collected and paired, resulting in 109,809 ECG-TTE pairs from 56,236 unique patients. The validation dataset consisted of 25,510 distinct TTE-ECG pairs (25,510 patients). Prevalence of LVEF≤40% and LVEF<50% was 5.4% and 7.9% respectively. The LVEF≤40% model demonstrated an AUC of 0.963 (95% CI: 0.959-0.966), sensitivity 0.924 (95% CI: 0.91-0.937), specificity 0.887 (95% CI: 0.883-0.891), and F1-score of 0.474 (95% CI: 0.457-0.490). PPV and NPV were 0.318 (95% CI: 0.304-0.333) and 0.995 (95% CI: 0.994-0.996) respectively. Performance of the LVEF <50% model shows an AUC of 0.952 (95% CI: 0.947-0.956), with a slightly lower sensitivity of 0.899 (95% CI: 0.886-0.912), specificity of 0.875 (95% CI: 0.871-0.879), PPV of 0.382 (95% CI: 0.368-0.395), NPV of 0.99 (95% CI: 0.989-0.992), and F1-score of 0.536 (0.521-0.55).
Conclusion
The smartphone-integrated AI model can reliably detect reduced LVEF from standard 12-lead ECGs. Our findings suggest these single 12 lead-ECG based models could serve as a point-of-care screening tool to identify such patients benefiting from further echocardiographic evaluation and consequent management acceleration.
Authors: Anthony Demolder, MD, MSc, PhD, Robert Herman, MD, PhD, Boris Vavrik, MSc, Michal Martonak, MSc, Vladimir Boza, MSc, PhD, Martin Herman, MSc, Timotej Paluš, MSc, Viera Kresnakova, MSc, PhD, Jakub Bahyl, MSc, Andrej Iring, MSc, Jozef Bartunek, MD, PhD, Marc Vanderheyden, MD, Ward Heggermont, PhD, MSc, MD, and Martin Penicka, MD, PhD