The sudden collapse of a top athlete in the middle of a game, often on live TV cameras, is usually accompanied by questions about the cause of this dramatic situation. The public is mostly mistakenly convinced that the athlete had a heart attack. However, the truth is that heart attacks rarely cause these life-threatening situations in young people.
The cause of the dramatic collapse of top athletes (but of course not only them), usually within seconds, is a severe sudden disturbance in the heart’s electrical activity – arrhythmia.
Why are young athletes collapsing: Understanding Arrhythmia and Heart’s Electrical Disturbances
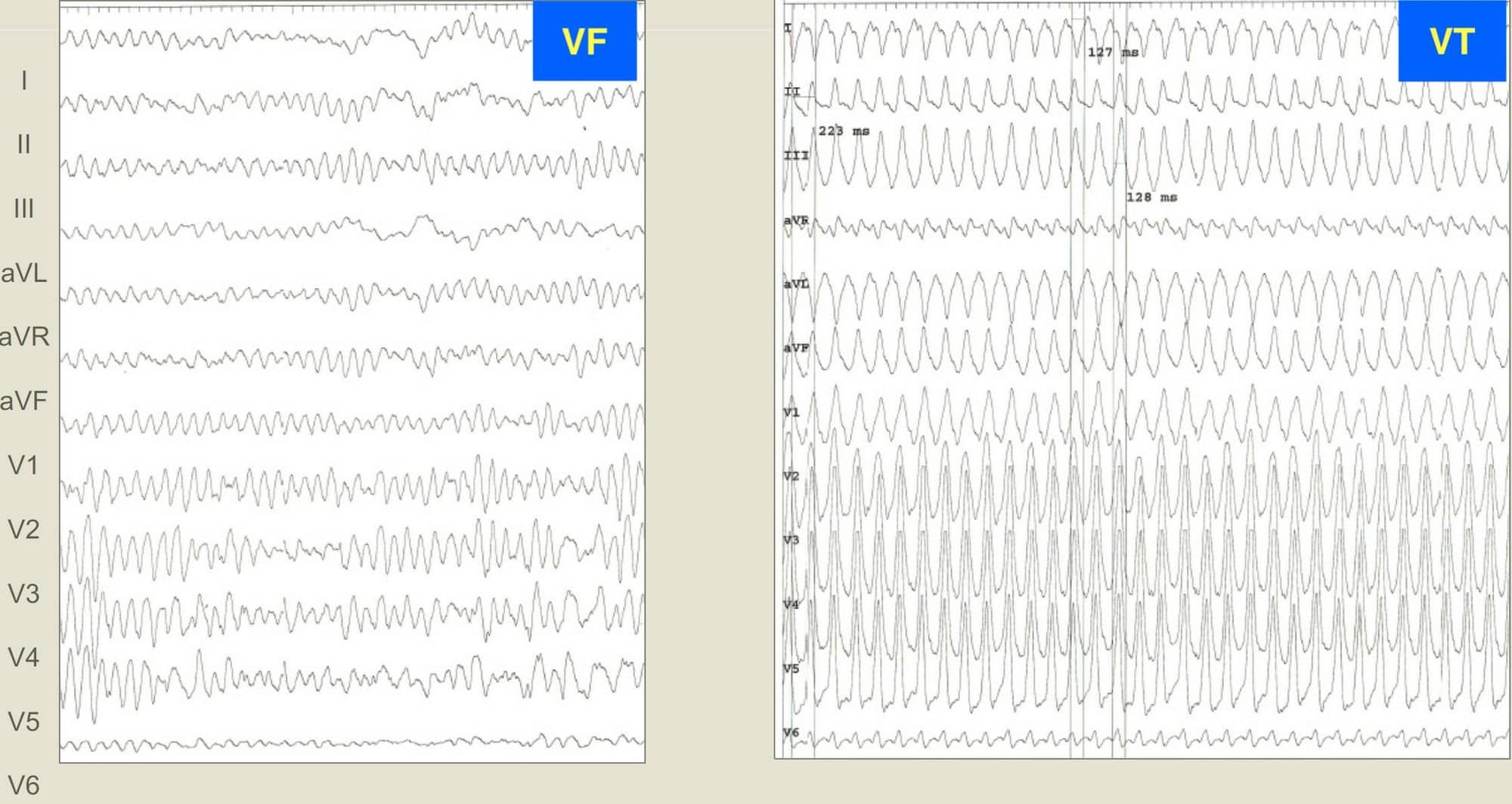
Arrhythmia is the creation of very fast chaotic electrical impulses reaching a frequency of around 300-400/minute, during which the pumping action of the heart stops, the blood stops flowing into the body, and we, therefore, speak of circulatory arrest. The brain is the first organ to react to this potentially fatal situation, and the patient loses consciousness.
Case Study: Damar Hamlin’s Near-Fatal Collapse
Even earlier this year, 24-year-old Buffalo Bills safety Damar Hamlin suddenly collapsed in the middle of an American football game. Following a routine tackle, he went into cardiac arrest. Thanks to the timely deployment of a defibrillator, he survived the arrhythmia and is on the mend now.
But why did it happen? There is no straightforward explanation – the occlusion of circulation can have many causes. Let us look at what we know about the heart’s electrical activity and how situations like the one happening to Mr Hamlin could be prevented.
The chaos of the heart’s electrical impulses can be deadly.
The heart is a muscular pump that pumps blood in parallel through 2 circuits – the “large” whole-body circuit and the “small” pulmonary circuit. The heart muscle alternately contracts and relaxes, sucking deoxygenated blood from the body and pushing it through the lungs through the right ventricle. After oxygenation, the blood returns to the left ventricle, which ejects it into the aorta and, from there, to the whole body.
A correctly timed electrical impulse conditions the correct function of the heart and its every contraction. Physiological electrical impulses arise in a cluster of special cells in the confluence of a large vein from the upper part of the body (the so-called superior vena cava) and the right atrium of the heart, which is called the sinus node.
The Electrical Symphony of the Heart
The sinus node creates electrical impulses with a frequency corresponding to the need for sufficient blood supply for the whole organism. This need is very variable and, depending on the load and the level of neurovegetative stimulation, it usually ranges from 50 to 200 impulses per minute in a young, healthy organism.
The electrical impulse is then distributed through a network of special cells that function as cables to all areas of the heart muscle. This activity ensures the synchronous contraction of the ventricles, which is necessary for optimal efficiency in expelling blood from the heart.
Stay on the pulse with our newsletter
Your submission was successful
Ventricular Fibrillation: A Lethal Arrhythmia
One of the disturbances in the heart’s electrical activity is the sudden appearance of several deposits in the muscle of the heart chambers, which begin to send uncoordinated high-frequency electrical impulses to their surroundings – 300-400 times per minute.
As a result, the heart begins to oscillate chaotically and immediately stops pumping blood – blood circulation stops. This type of malignant arrhythmia is called ventricular fibrillation – the most common cause of sudden cardiac death.
Note that ventricular fibrillation fundamentally differs from atrial fibrillation, a common, often asymptomatic arrhythmia affecting 3% of the adult population.
If the ventricular fibrillation is not treated within a few minutes, irreversible damage occurs, and gradually all organs fail. First is the brain, the most sensitive organ to oxygen deprivation.
Athletes Collapsing: How Can a Fatal Pathological Process Be Reversed?
Averting the fatal end of someone suffering from ventricular fibrillation presupposes restoring the correct electrical function of the heart as soon as possible – i.e., eliminating electrical chaos. Applying an electrical discharge with several hundred volts and a short millisecond duration can achieve this most effectively.
Such a discharge induces an electrical “reset” of the heart – the entire heart contracts at once with a powerful discharge. There is a brief electrical silence, and regular electrical activity is restored with the return of blood circulation.
Reversing the Fatal Process: The Role of Defibrillation
However, to apply such an “electric shock,” it is necessary to have a special device – a defibrillator.
Ideally, a defibrillator should be brought to a victim of ventricular fibrillation within a few minutes. Since a defibrillator is typically available at the sports field, the chance to save an athlete who suffered cardiac arrest during a sporting event is generally relatively high. In real life, waiting for a defibrillator usually takes much longer – often tens of minutes after which the chance for patient survival is minimal.
While waiting for a defibrillator, a patient must be given proper resuscitation. Their survival depends on it. After securing the airways (preventing the tongue-swallowing), its essence is a powerful rhythmic chest compression at the sternum level with both palms placed on top of each other.
The Crucial Window for Action
The compression speed should be about 100 compressions per minute – this is approximately the rhythm of the well-known Bee Gees song with a very fitting name, “Stayin’ Alive”. With correctly applied compression of sufficient force, a rib or ribs may break (often audibly), but it is a negligible complication in this situation.
If an electric defibrillation shock with the restoration of blood circulation is timely applied, bridged by proper resuscitation, we are talking about an averted sudden death. In general, without providing resuscitation manoeuvres, the victim’s probability of survival decreases by 10% with each passing minute, so after 10 minutes of untreated ventricular fibrillation, the patient usually dies.
Several scientific works have convincingly proven that correct and timely resuscitation by laypeople by witnesses of the event is a decisive factor in averting sudden death and surviving the patient without brain damage.
A fight against time
After a nationwide campaign on proper resuscitation in Denmark, the survival rate of patients after sudden circulatory arrest increased 4-fold to more than 30%.
However, first aid must be completed as quickly as possible using an automated external defibrillator (AED). These are most often located in places with a high density and movement of people (transport hubs, sports fields, shopping centres, hotel lobbies, etc.).
Delayed arrival of the emergency medical service, whether due to late contacting its dispatch or due to the poor condition of the road network and heavy traffic in cities, can be fatal for the patient.
In some areas of Sweden, trials have begun to use drones controlled by the rescue centre to transport the defibrillator to the victim. However, for the rescue operation to start at all, it is vitally important to immediately inform the dispatch of the rescue service about the case.
Despite timely delivery of defibrillation, circulation cannot always be successfully restored, and the heart fails to return to normal electrical function. In these situations, highly specialised assistance with oxygen administration, airway intubation, intravenous drug administration, or extracorporeal circulation support and cooling of the patient is required.
Why ventricular fibrillation occurs – young heart vs. old heart
The causes of sudden arrhythmic death vary greatly, depending on the patient’s age. However, sudden death at a young age is, for understandable reasons, perceived more dramatically than in a person who has been receiving heart treatment for years.
For a layperson, it may seem incomprehensible how such a severe condition can occur in a person representing the very symbol of physical health – a top athlete – who also undergoes periodic preventive medical examinations by sports doctors.
However, such life-threatening sudden events with much media attention are relatively rare, occurring in approximately one in 15,000 athletes per year, significantly less than in the “non-athletic” population.
From a global perspective, sudden cardiac death accounts for approximately 15% of all deaths, a significant mortality rate.
The conducted studies of victims of sudden cardiac death show two types of diseases that young people, including athletes, typically suffer from:
The first group of diseases
Primary electrical diseases of the heart are most often a result of genetic mutations, of which we still know only a fragment. Gene mutations cause, under certain circumstances, abnormal permeability of ions through the membranes of some heart cells, which causes the abnormal spontaneous electrical activity of these cells, which sets off “electrical fireworks” in the heart.
The malfunction can only occur under certain circumstances, e.g. during extreme heart stimulation with adrenaline, under the influence of doping, at a high environmental temperature (e.g. a hot bath), or after using drugs.
Such a genetic disorder cannot be detected during a routine preventive examination. An electrocardiogram (ECG) at rest and during exercise and an ultrasound examination of the heart can be completely normal. However, essential data towards the correct diagnosis can be, e.g., sudden death under the age of 50 in blood relatives or dropping out in childhood.
The second group of diseases
The primary genetically determined disease of the heart muscle is the so-called hypertrophic cardiomyopathy. At a young age, this can be manifested only by a relatively insignificant thickening of the heart’s walls, which, however, also occurs physiologically in athletes as a result of their high level of training. A genetic examination supplemented by a magnetic resonance heart examination can be decisive.
Younger age groups: The case of an American football player
When it comes to Damar Hamlin, the above-mentioned football player, what was probably the case was an underestimated mechanism of arrhythmia – the player collapsed after a sudden collision with another player who hit him in the chest with his helmet while running.
When a hard object strikes the chest in sports, such as a baseball or basketball, the mechanical energy of the impact can be converted into an electrical impulse, which can disrupt the heart’s rhythm and trigger a fatal arrhythmia, even in those with perfectly healthy hearts.
This occurrence is the so-called ‘concussion of the heart’, in Latin commotio cordis, a somewhat archaic name still used in some professional literature. This mechanism can also be triggered when the chest hits the steering wheel in a traffic accident.
Higher age groups
In the older-adult category (over 50 years of age), the most common cause is acute lack of blood supply to the heart muscle – ischemia – due to the closure of the blood flow in the large arteries that supply the heart. Atherothrombosis is typically the reason for artery closure. Fat deposits cause an artery’s narrowing; subsequently, a blood clot forms and blocks the vessel like a plug. In some cases, arrhythmia – ventricular fibrillation – occurs within seconds, which kills the patient even before the heart attack develops, i.e. the heart muscle dies.
Nowadays, most patients survive a heart attack but are left with a scar of varying sizes on their hearts. Such a chronic scar is the most common cause of a slightly different but potentially fatal arrhythmia in people after a heart attack – the arrhythmia is called ‘ventricular tachycardia‘.
In ventricular tachycardia, the impulses are initially more organised than in ventricular fibrillation and usually have a lower frequency, typically in the range of 160-240 impulses per minute. The patient does not always lose consciousness immediately. However, without treatment, such an arrhythmia usually degenerates into chaotic ventricular fibrillation with a life-threatening outcome within a few minutes. Timely use of the defibrillator is again crucial for the patient’s survival.
In the case of post-infarction arrhythmias, ventricular tachycardia triggers an electrical impulse that “circulates” in the scar tissue caused by the infarction. In this case, we can suppress the arrhythmia by successfully “burning” this part of the scar with a catheter through which we apply a high-frequency electric current (microwave principle). This method is referred to as catheter ablation.
The method can also be used in patients in whom an abnormal electrical impulse (which always originates from one or a few cell clusters on the inner surface of the heart’s chambers) causes ventricular fibrillation. By eliminating these cell clusters, we remove the arrhythmia trigger.
Untreated high blood pressure
A heart damaged by untreated high blood pressure is also a critical terrain for these arrhythmias. With increasing age, the heart – apart from ageing – is often simultaneously affected by several pathological processes, significantly increasing the risk of sudden cardiac death.
In current-state cardiology, it is possible to identify some patients with such a risk and implant a special generator of electric impulses – a defibrillator – under the skin in the chest area. It is a compact device in shape and size, similar to a classic pocket watch, weighing around 70 grams. Here’s schema of an implantable defibrillator (ICD) in the area below the left collarbone with electrodes inserted into the heart:
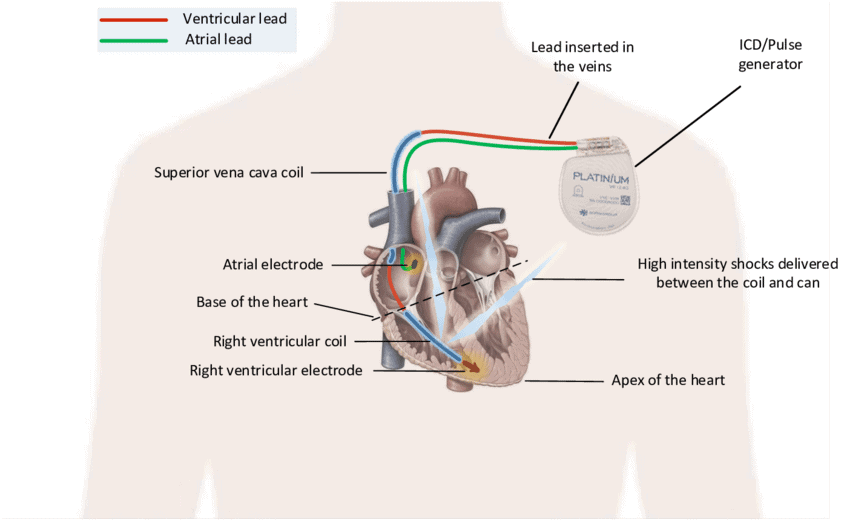
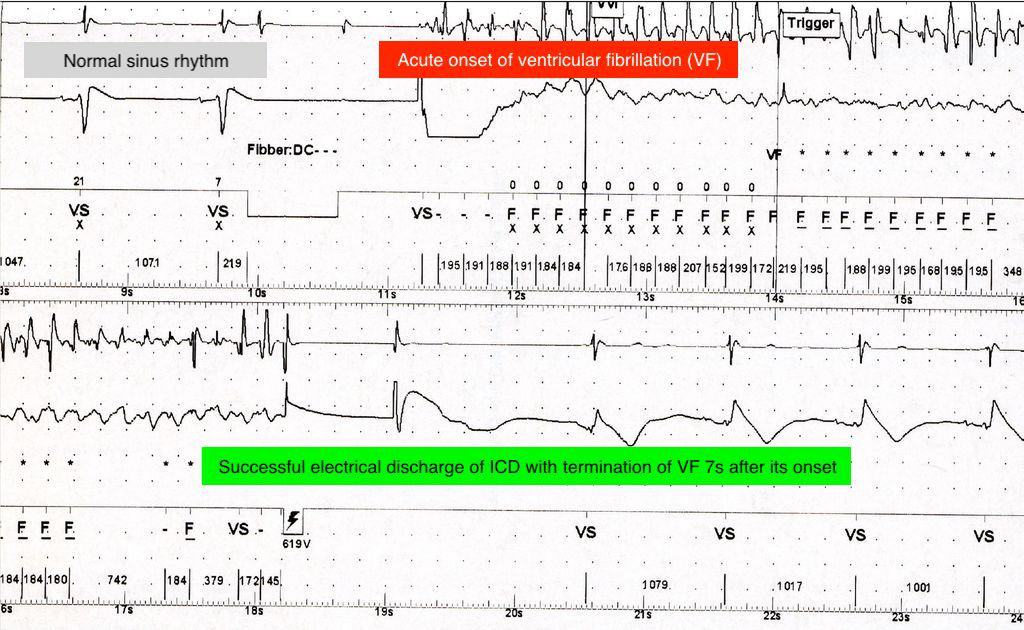
The device continuously monitors the electrical activity of the heart. In ventricular tachycardia or fibrillation, the device recognises the arrhythmia and terminates it within a few tens of seconds with a series of electrical impulses or a discharge of 40-80J (Image 2).
Can the potentially fatal collapses of athletes be prevented?
It is practically impossible to carry out preventive, highly specialised and expensive genetic and imaging examinations in millions of otherwise healthy people who want to do sports.
Although sudden cardiac arrests due to arrhythmia are rare in athletes compared to the rest of the population, they always attract the media’s attention and, thus, the entire public. Unfortunately, as it often happens, the first and only manifestation of the disease is a collapse in the sports field. If the sportsman/sportswoman survives the sudden cardiac death, the current special field of cardiology – arrhythmology – can help them further.
A real-life example is the case of 29-year-old Danish football player Christian Eriksen, who survived sudden cardiac arrest during an international match in 2021 and today, with an implanted defibrillator, continues his career as a football player for Manchester United.
Despite periodic examinations of top athletes, we are unlikely to detect all at-risk individuals in time in the foreseeable future. Sadly, this is why we will probably keep witnessing such dramatic cases.
However, the explosive development of artificial intelligence brings some optimism. First, in the advanced cardiac screening of large populations. Second, in analysing the electrocardiogram (ECG) using deep learning (deep learning is a form of machine learning using computer neural networks).
An AI-powered ECG analysis can identify previously undetected or overlooked content of an ECG recording, providing an unprecedented opportunity for early detection of the risk of developing life-threatening arrhythmias.