Overview
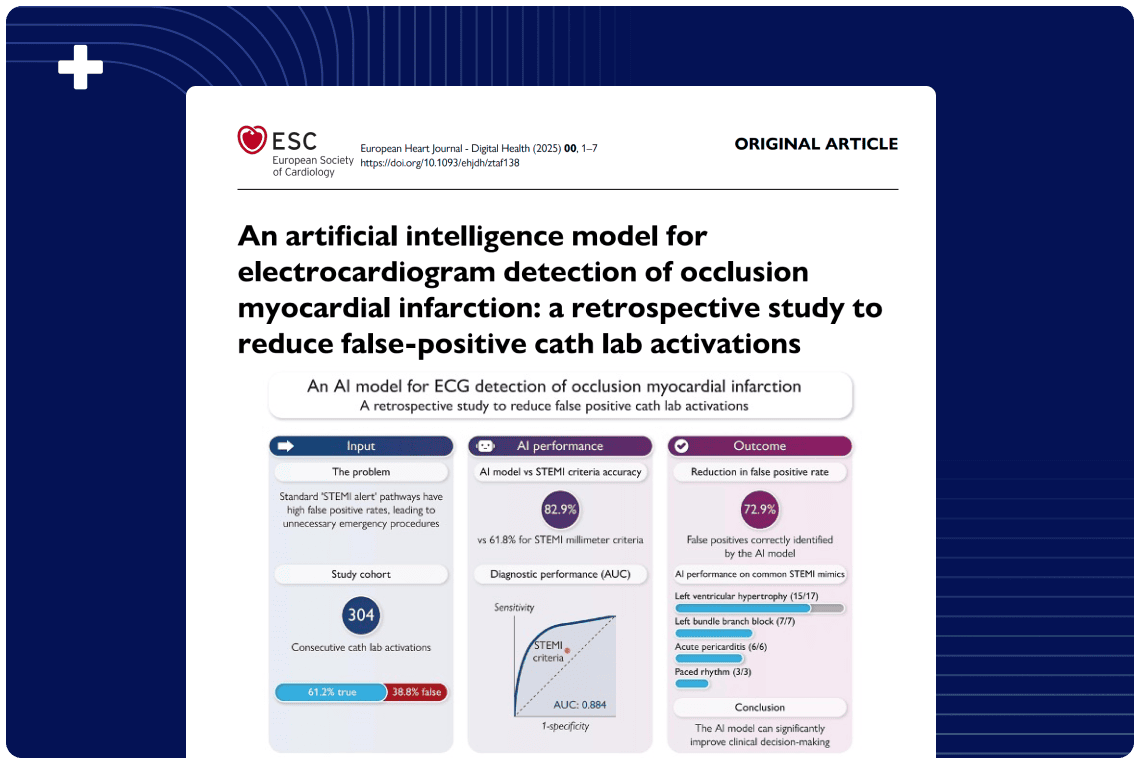
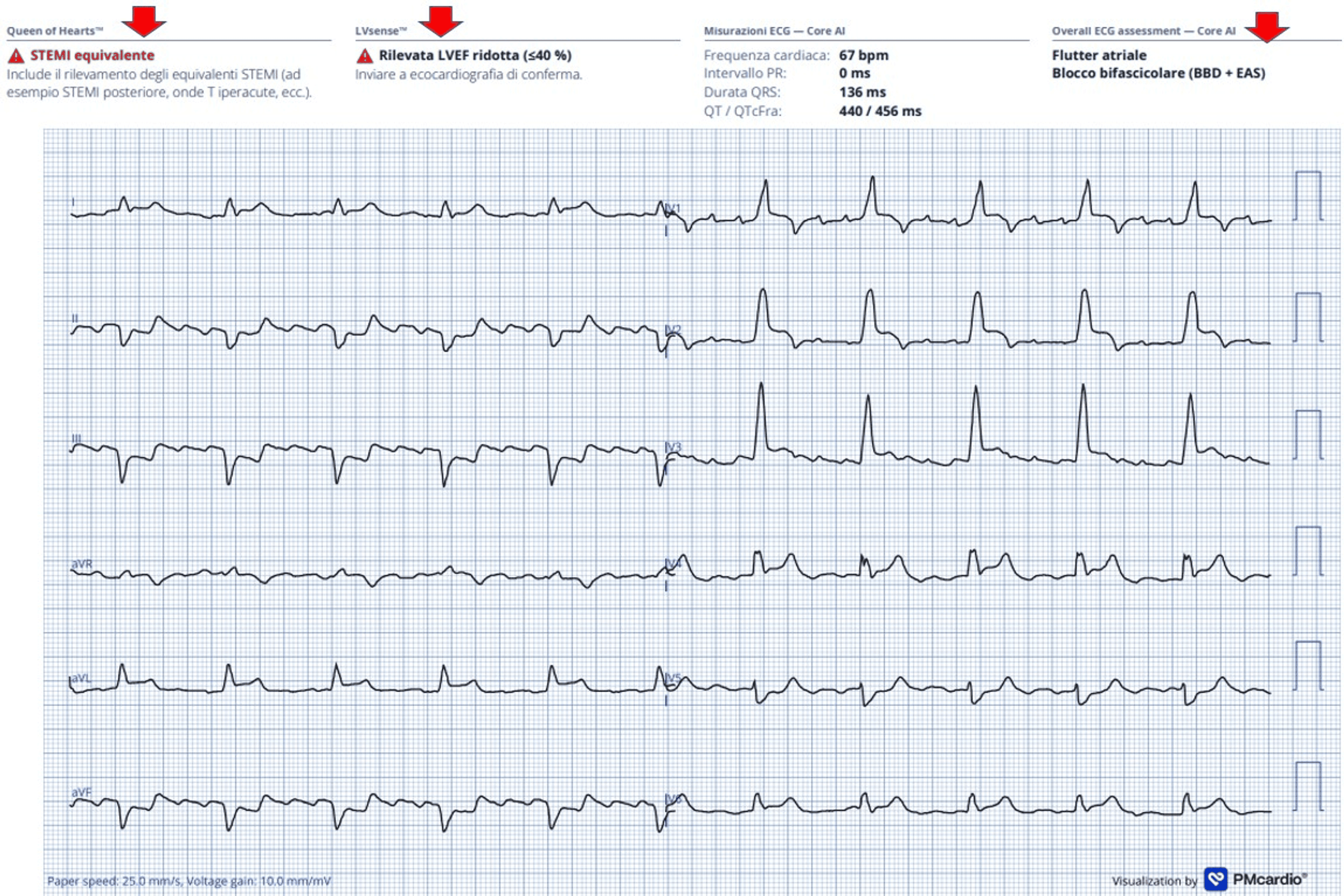
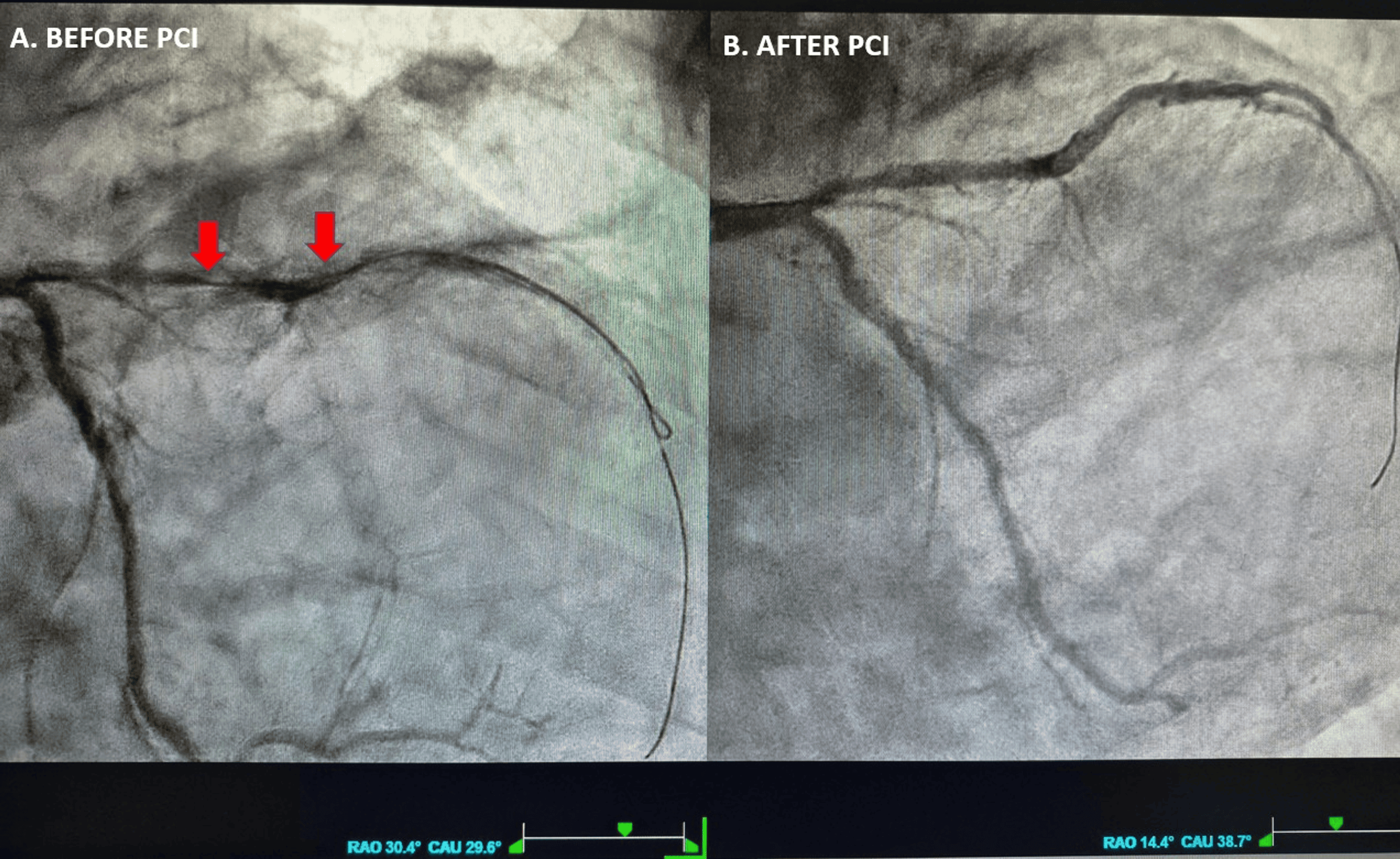
This single-patient case report describes an elderly man presenting with chest pain, hypotension, and bifascicular block (BFB)—a combination of right bundle branch block (RBBB) and left anterior fascicular block (LAFB)—whose ECG showed QRS‑concordant anterior and lateral ST‑segment elevation consistent with a STEMI‑equivalent / occlusive myocardial infarction (OMI) pattern. Urgent coronary angiography revealed a long, severely calcified, near‑occlusive proximal left anterior descending (LAD) artery lesion, successfully treated with primary PCI and drug‑eluting stent implantation, achieving TIMI 3 flow. The Queen of Hearts (PMcardio) AI‑based smartphone app correctly classified the ECG as STEMI‑equivalent, identified atrial flutter and BFB, and predicted reduced left ventricular ejection fraction, later confirmed by echocardiography (EF 38%). This case highlights BFB with concordant anterior ST elevation as a high-risk marker of proximal LAD culprit OMI and provides anecdotal evidence that specialized AI-enabled ECG interpretation can support rapid and accurate decision-making in ACS.
Published in: Cureus
Published on: 26 November 2025
Background
Accurate recognition of occlusive myocardial infarction in the presence of conduction disturbances remains challenging. While current ESC guidelines acknowledge bundle branch blocks as important in ACS, they do not specifically define bifascicular block (RBBB + LAFB) as a STEMI‑equivalent, despite its association with proximal LAD or left main occlusion, extensive myocardial injury, heart failure, and increased mortality. In parallel, AI-powered ECG tools, such as Queen of Hearts, aim to go beyond simple ST-elevation thresholds to detect STEMI-equivalent/OMI patterns and estimate ventricular function, potentially reducing both missed OMI cases and unnecessary cath-lab activations.
Methods
This single‑case report describes a 77‑year‑old man with multiple cardiovascular comorbidities evaluated by emergency medical services for prolonged chest pain. Serial 12-lead ECGs were obtained and interpreted by clinicians, and then processed using the Queen of Hearts (PMcardio) smartphone app, which analyzed rhythm, conduction, ST-T patterns, and predicted left ventricular ejection fraction. The patient underwent emergent coronary angiography and primary PCI of the culprit lesion. The diagnostic work-up included laboratory testing (cardiac biomarkers, renal function, and lipid profile) and transthoracic echocardiography on the day after PCI to quantify wall-motion abnormalities and systolic function, followed by guideline-directed medical therapy and short-term clinical follow-up.
Results
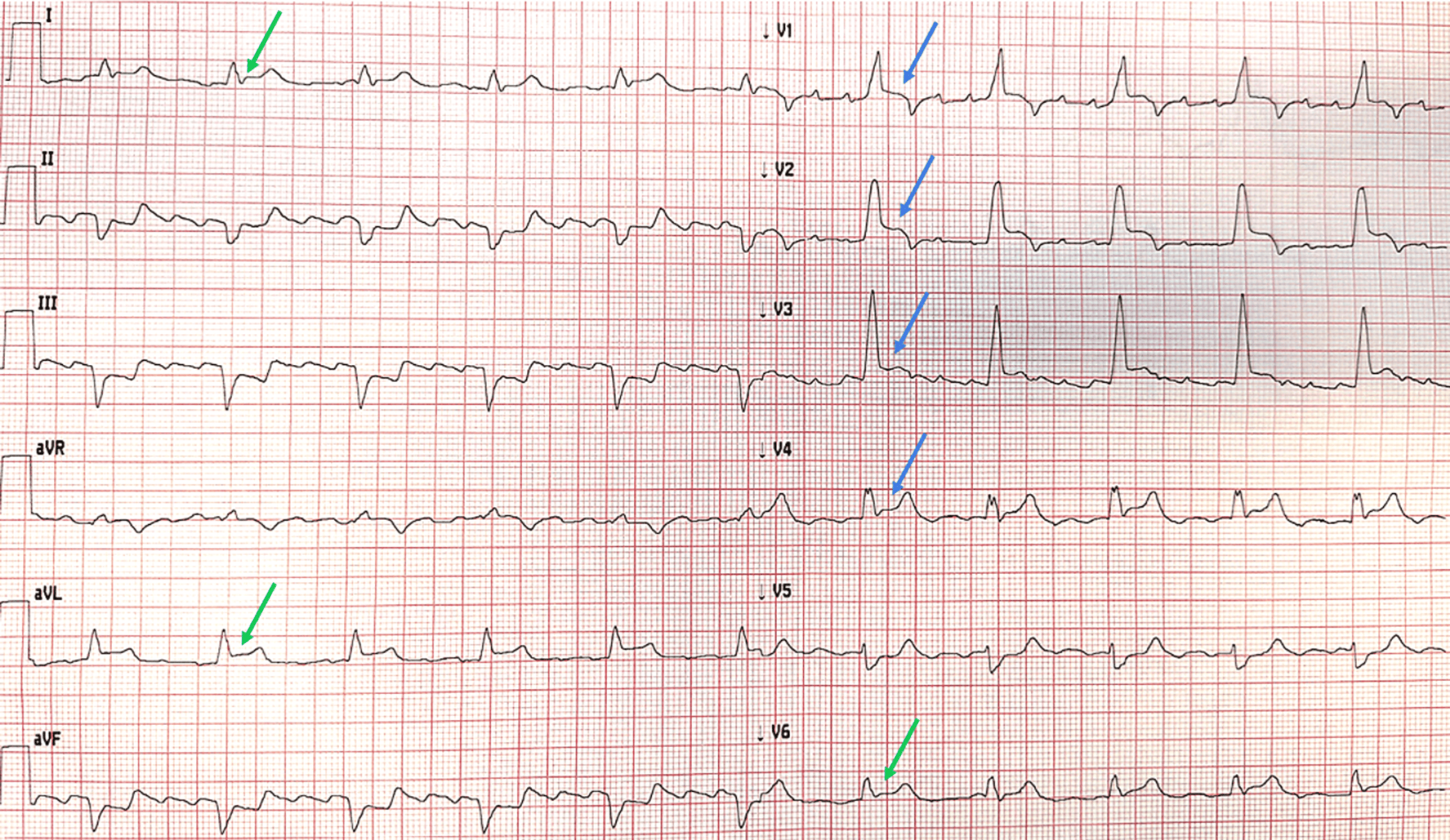
The initial ECG (page 2) showed atrial flutter with 4:1 AV conduction, complete RBBB, LAFB, and QRS‑concordant ST‑segment elevation in V1–V4 with additional lateral ST elevation (I, aVL, V6) and reciprocal inferior changes, leading to a working diagnosis of anterolateral STEMI in the context of new or presumably new BFB. A second ECG (page 3) demonstrated further progression of anterior ST elevation. The Queen of Hearts app labeled the tracing as STEMI‑equivalent, detected the bifascicular block and atrial flutter, and predicted an EF <40%. Coronary angiography (page 4 and Video 1) revealed a severely calcified, near‑occlusive proximal LAD stenosis, treated successfully with drug‑eluting stent implantation and restoration of TIMI 3 flow; other coronary vessels showed only mild, non‑obstructive disease. Post‑PCI ECG (page 5) showed persistence of BFB but resolution of ST elevation with QRS‑discordant T‑wave changes typical for RBBB. Laboratory testing demonstrated markedly elevated high‑sensitivity troponin I and NT‑proBNP with moderate anemia and chronic kidney disease (Table 1, page 6). Echocardiography (Video 2) confirmed apical akinesia, anterior/anteroseptal hypokinesia, EF 38%, biatrial enlargement, and moderate ischemic mitral regurgitation, consistent with the AI‑predicted LV dysfunction. The in-hospital course was uncomplicated, and the patient was discharged after eight days on optimized heart failure and antithrombotic therapy.
Conclusion
In the appropriate clinical context, bifascicular block (RBBB + LAFB) with QRS‑concordant ST elevation in V1–V3 should be regarded as a STEMI‑equivalent pattern, strongly suggestive of proximal LAD‑culprit OMI and warranting immediate invasive evaluation and reperfusion. This case illustrates how the prompt recognition of this high-risk ECG presentation enabled timely PCI and how the Queen of Hearts AI application provided accurate, point-of-care confirmation of OMI and left ventricular dysfunction. Although AI‑based ECG tools appear promising adjuncts for real‑time ACS triage, they should complement rather than replace expert ECG interpretation and clinical judgment, and their broader performance must be validated beyond single‑case experience.
Authors: Lucio Giuseppe Granata, Francesco Russo, Simona Giubilato, Marilena Scarabelli, Francesco Amico