In the critical landscape of cardiac emergency care, early detection and accurate diagnosis of myocardial infarction (MI) are paramount for enhancing patient survival and outcomes1. The established criteria for diagnosing an ST-segment elevation myocardial infarction (STEMI) have been foundational in guiding healthcare professionals in emergency cardiovascular care for several decades2.
The criteria require the observation of the ST-segment elevation at the J point in two contiguous leads, requiring the elevation to measure at least 2.5 mm (0.25 mV) in men under 40 years of age, 2 mm (0.2 mV) in men aged 40 years and older, or 1.5 mm (0.15 mV) in women in leads V2–V3, and/or at least 1 mm (0.1 mV) in other contiguous chest leads or the limb leads3.
Table of Contents
STEMI Criteria and Its Limitations
A variety of ECG presentations diverge from this classic ST-segment elevation pattern yet still indicate acute myocardial ischemia4. Termed STEMI equivalents, these divergent patterns require the same level of urgency and treatment as traditional STEMIs, presenting a significant challenge for healthcare professionals to quickly identify and respond to these less obvious indicators of cardiac crises5. This foundation, coupled with ever-evolving research and a deepening understanding of MI ECG patterns, compels clinicians to continually adapt and broaden their diagnostic vigilance6.
STEMI diagnosis based on ECG findings is a critical step in the rapid initiation of life-saving interventions. However, the strict adherence to traditional STEMI criteria may lead to significant oversight of MI cases that do not exhibit classic ECG patterns. This oversight underscores the necessity for a broader understanding and recognition of STEMI equivalents among healthcare providers. By expanding our diagnostic lens beyond traditional criteria, we can ensure that a wider range of patients receive the timely care they need.
STEMI Equivalents: Play It Safe with Certified AI
- 2x higher sensitivity in occlusive MI detection
- 3h faster time to diagnosis
- Medical Device Class II(b) EU MDR CE-mark
- 5 FREE ECGs/month - no credit card needed
A Comprehensive Look at STEMI Equivalents
STEMI equivalent patterns play a crucial role in the diagnosis and treatment of acute coronary syndromes, signaling serious but manageable heart conditions often missed by traditional criteria7. Below, we explore some of the key STEMI equivalents, highlighting their diagnostic features and clinical implications.
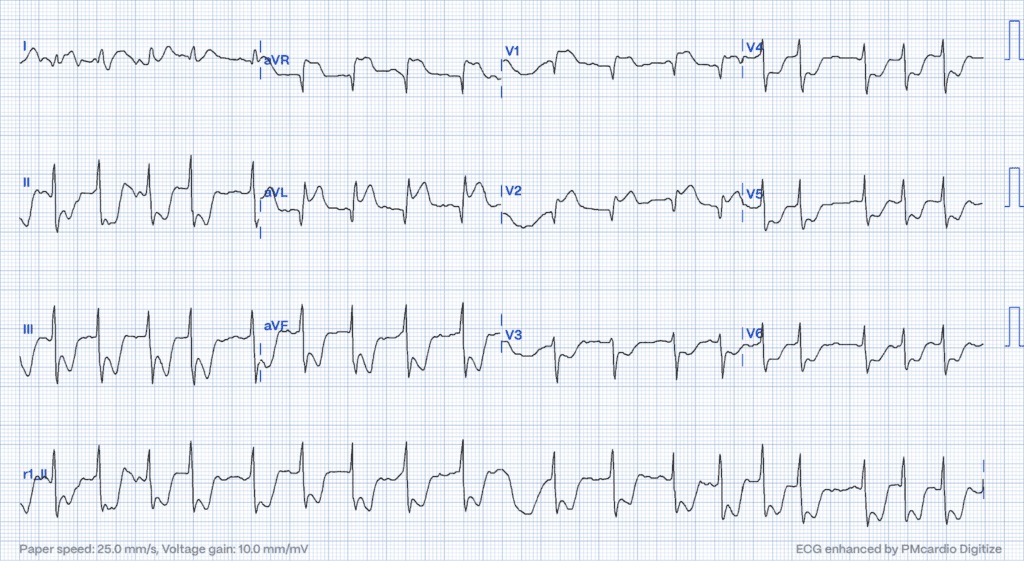
Sgarbossa’s Criteria: Diagnosing MIs in Bundle Branch Blocks and Ventricular Paced Rhythms
Sgarbossa’s Criteria are pivotal in diagnosing myocardial infarction (MI) in patients with left bundle branch block (LBBB) or those with ventricular paced rhythms5. These criteria have been further enhanced by the Smith-modified Sgarbossa criterion a refinement that evaluates the proportion of ST elevation relative to the depth of the S wave, thereby improving the accuracy of MI detection11.
Sgarbossa’s Criteria include:
- Concordant ST Elevation: ST elevation of 1 mm or more in leads with a positive QRS complex is a strong indicator of MI, scoring 5 points. This concordance signifies that the direction of the ST segment elevation aligns with the QRS complex5.
- Concordant ST Depression: This is noted when there’s an ST depression of 1 mm or more in leads V1, V2, or V3, scoring 3 points. Within the context of Sgarbossa’s Criteria, concordant ST depression in these chest leads is particularly indicative of posterior MI12. This criterion is essential, distinguishing it from global ST depression patterns, which may point to more extensive ischemia or other conditions like pericarditis.
- Excessively Discordant ST Elevation: Elevation of 5 mm or more in leads with a negative QRS complex receives 2 points. While some discordance is expected in LBBB, excessive elevation is suggestive of ischemia5.
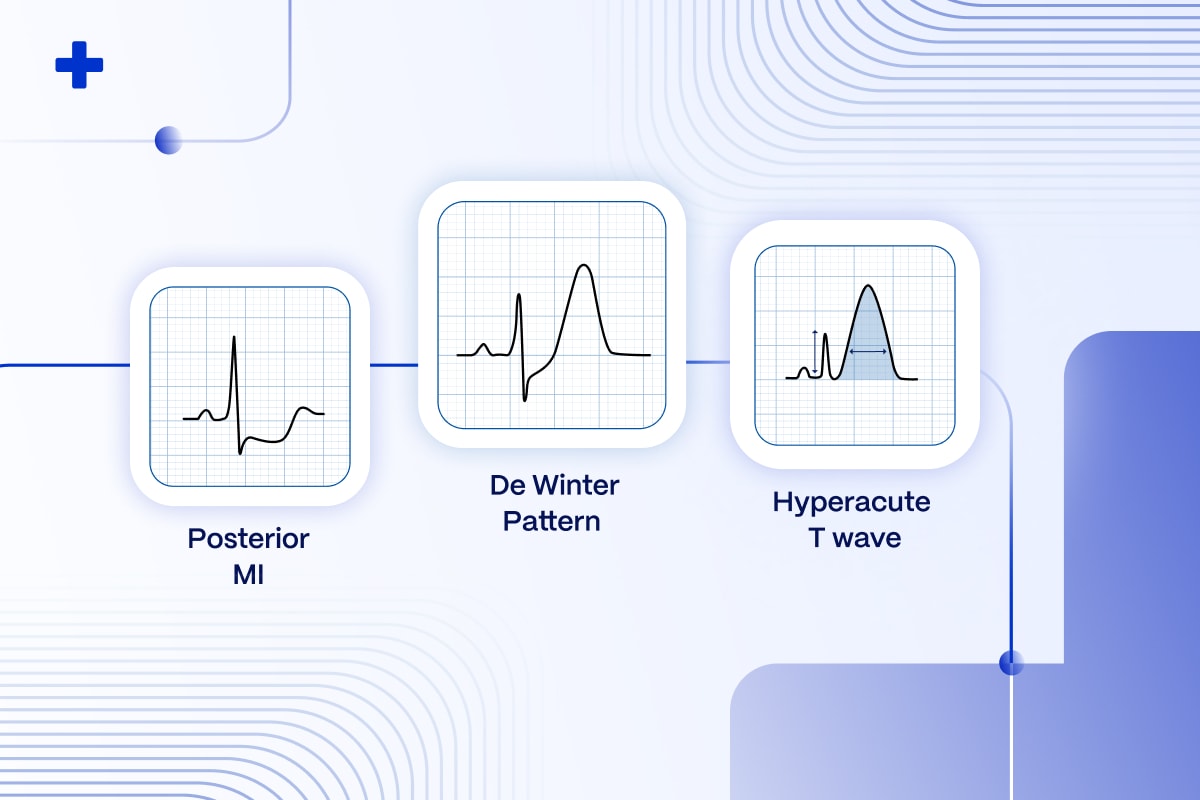
Hyperacute T-waves: Early Indicators of Ischemia
Marked by their tall, peaked appearance, hyperacute T-waves emerge as the initial ECG sign of myocardial ischemia. Predominantly observed in the precordial leads, these waves underscore the urgency of early intervention to mitigate myocardial damage13.
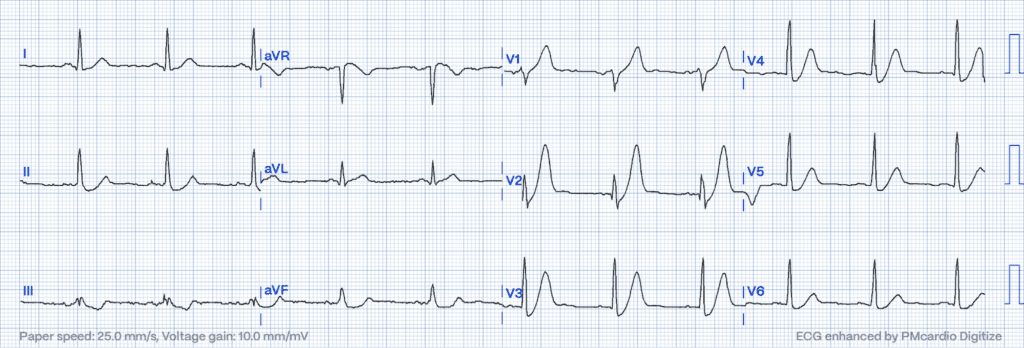
De Winter’s T-waves: Signaling Proximal LAD Occlusion Without ST Elevation
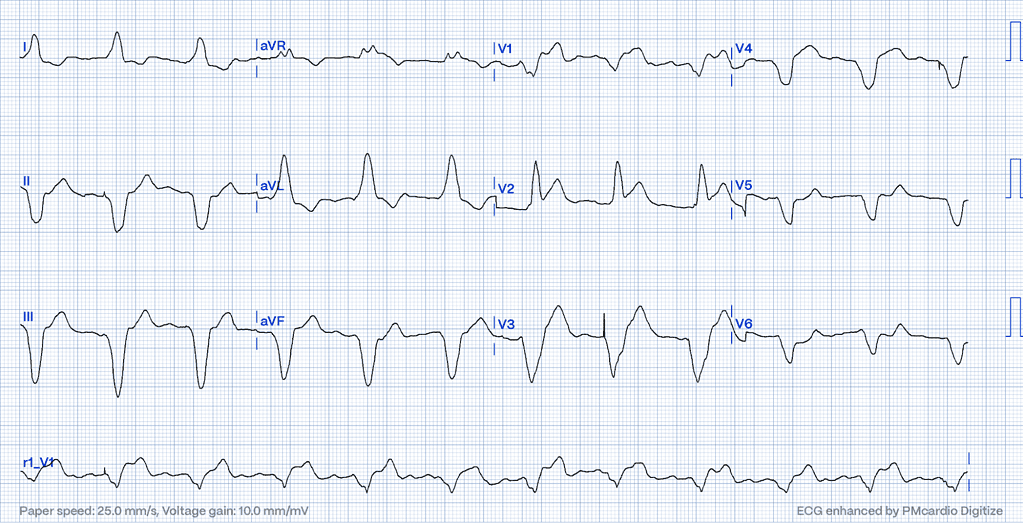
Unique to De Winter’s pattern are upsloping ST-segment depressions at the J point in precordial leads, transitioning into tall, symmetrical T-waves. Absence of typical ST elevation notwithstanding, this pattern suggests a proximal LAD occlusion, demanding prompt revascularization10.
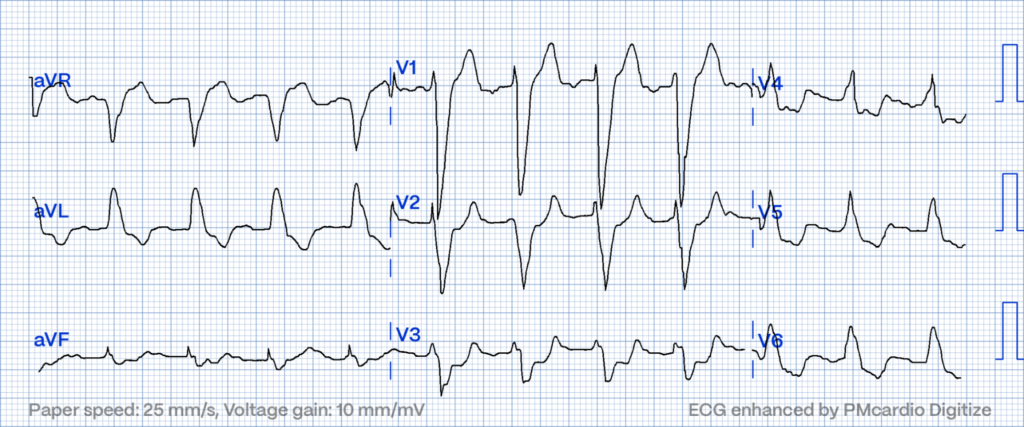
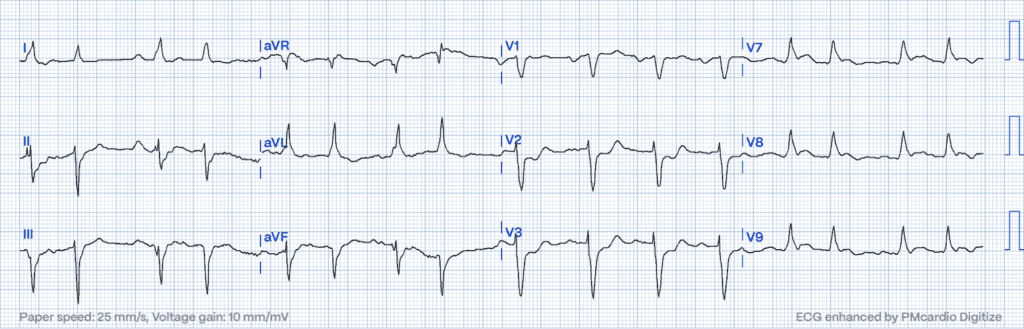
Posterior MI: Uncovering the Concealed Threat
Posterior MI presents a diagnostic challenge, often revealing itself through indirect signs on a standard ECG14, such as horizontal ST depression and tall, broad R waves in the anterior leads. Its stealthy nature necessitates vigilance and sometimes additional posterior leads for accurate identification.
Isolated ST Elevation in aVR: Marking Global Ischemic Risk
An isolated elevation in lead aVR, alongside widespread ST depression, could signify a severe obstruction in the left main coronary artery or extensive subendocardial ischemia15. This pattern flags a high risk of widespread myocardial danger, meriting immediate attention.
Each of these STEMI equivalents enriches the diagnostic toolkit, enabling clinicians to identify and treat a broader array of acute coronary syndromes. Their recognition not only challenges but also expands the clinical understanding of MI, underscoring the complexity and diversity of cardiac emergencies.
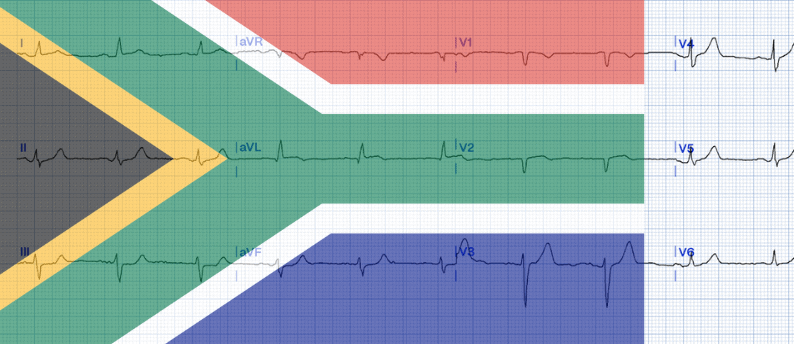
South African Flag Sign: Tracing the Shadow
The South African flag sign (SAFS) is a notable ECG finding, requiring immediate clinical attention17.
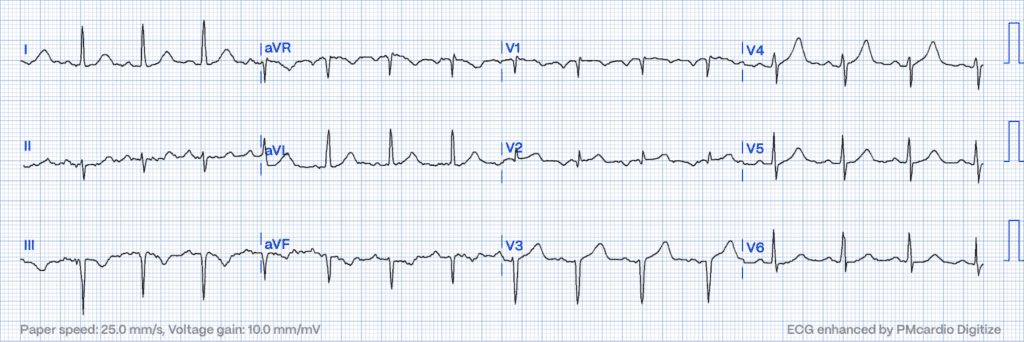
High lateral STEMI is linked to a specific ST elevation pattern resulting from the acute blockage of the first diagonal branch of the LAD artery (LAD-D1). This condition manifests on the 12-lead ECG, which is typically displayed in a 4×3 format, where the most notable ST changes mimic the design of the South African flag:
- ST Elevation is observed in Lead I, aVL, and V217.
- ST Depression is noted in Lead III (as well as other inferior leads)17.
Occlusion of the left circumflex artery may lead to elevation of the ST-segment in leads I and aVL, as well as in leads V5 and V6.
Is Wellens Syndrome a STEMI Equivalent?
Despite widespread belief, Wellens’ Syndrome does not classify as STEMI equivalents. It represents a reperfusion phenomenon rather than a sustained, complete coronary occlusion. In Wellens’ syndrome, specific ECG patterns, notably biphasic or deeply inverted T waves in the precordial leads, alert clinicians to severe but reversible ischemic injury due to partial reperfusion of the LAD artery. To take a deeper dive into the topic, explore the hallmarks of Wellens’ syndrome and its ECG pattern here:
Wellens’ Syndrome: Are You Prepared to Prevent Acute Coronary Occlusions?
While the urgency of management may parallel that of STEMI, the underlying mechanisms and therapeutic targets differ, emphasizing early diagnosis and proactive treatment to prevent progression rather than responding to an established infarction.
STEMI equivalents: Emerging Patterns
The conversation around MI is evolving with the recognition of Occlusion Myocardial Infarction (OMI), a term that encompasses both classic STEMI and its equivalents16. OMI highlights the need for a paradigm shift in our diagnostic approach, focusing on the pathophysiological basis of occlusion itself, rather than solely on ECG patterns18.
The distinction between OMI and STEMI lies in the broader inclusion of occlusive coronary events under the OMI umbrella, regardless of their ECG presentation10. This perspective compels healthcare professionals to integrate clinical symptoms and supplemental imaging or diagnostic evaluations into their assessments, guaranteeing that patients experiencing occlusive events are afforded appropriate care, even in instances where traditional STEMI criteria are not satisfied16.
Bridging the Gap with Enhanced Diagnostic Tools
The latest insights from the European Society of Cardiology (ESC) Congress have marked a transformative shift in both the comprehension and handling of Acute Coronary Syndrome (ACS), steering us towards embracing a more encompassing OMI criteria via STEMI equivalents. This evolution reflects a recognition of ACS as a spectrum, bridging the traditional STEMI/NSTEMI classifications to a more nuanced approach that acknowledges the dynamic and diverse presentations of coronary occlusion.
Notably, the integration of STEMI equivalents into this framework highlights the need for a diagnostic strategy that transcends conventional ECG interpretations, aligning with the underlying pathology rather than the initial screening tool’s limitations.
As we navigate through these advancements, the introduction of the OMI paradigm signifies a crucial development in clinical practice, emphasizing the need for detailed diagnostics in managing acute coronary syndromes (ACS)2. The transition to a spectrum-based understanding of ACS, augmented by cutting edge technologies represents a major advancement in cardiovascular medicine, offering a future where patients receive timely, precise, and tailored treatment strategies.
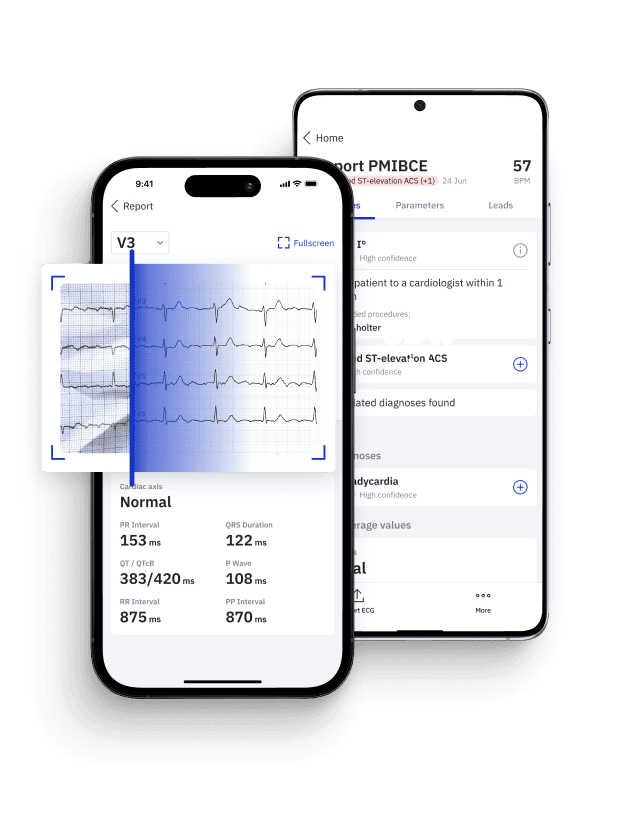
PMcardio embodies the integration of the OMI paradigm into clinical practice, offering healthcare providers a comprehensive solution that enhances diagnostic precision and patient care17.
Conclusion on STEMI Equivalents: Embracing the Full Spectrum for Comprehensive Care
The acknowledgment of STEMI equivalents and the broader Occlusion MI concept represents a substantial advancement in cardiovascular medicine17. This evolution encourages a broader diagnostic perspective and therapeutic approach, supported by technological innovations. The PMcardio platform aids healthcare professionals in navigating the complexities of cardiac events, ensuring timely and accurate care. By adopting such integrated tools, the potential to significantly enhance patient outcomes is realized, demonstrating a commitment to leveraging all resources for superior care delivery and patient-centered approaches.
Pin Down STEMI Equivalents with Certified AI
- Medical Device Class II(b) EU MDR CE-mark
- 2x higher sensitivity in occlusive MI detection
- 3h faster time to diagnosis
- 5 FREE ECGs/month - no credit card needed
References
- Libby P, et al. Mechanisms of acute coronary syndromes and their implications for therapy. N Engl J Med. 2013;368:2004-2013.
- Thygesen K, et al. Fourth Universal Definition of Myocardial Infarction (2018). J Am Coll Cardiol. 2018;72(18):2231-2264.
- Amsterdam EA, et al. 2014 AHA/ACC Guideline for the Management of Patients With Non–ST-Elevation Acute Coronary Syndromes. J Am Coll Cardiol. 2014;64(24):e139-e228.
- Kosuge M, Kimura K, Ishikawa T, Ebina T, Hibi K, Tsukahara K, et al. Differences between men and women in terms of clinical features of ST-segment elevation acute myocardial infarction. Circ J. 2006;70(3):222-6.
- Sgarbossa EB, et al. Electrocardiographic Diagnosis of Evolving Acute Myocardial Infarction in the Presence of Left Bundle-Branch Block. N Engl J Med. 1996;334(8):481-487.
- de Winter RJ, et al. A New ECG Sign of Proximal LAD Occlusion. N Engl J Med. 2008;359(19):2071-2073.
- Rokos IC, French WJ, Mattu A, Nichol G, Farkouh ME. Appropriate Cardiac Cath Lab Activation: Optimizing Electrocardiogram Interpretation and Clinical Decision Making for Acute ST-Elevation Myocardial Infarction. Am Heart J. 2010;160(6):995-1003. doi:10.1016/j.ahj.2010.08.011.
- de Zwaan C, Bär FW, Wellens HJ. Characteristic electrocardiographic pattern indicating a critical stenosis high in left anterior descending coronary artery in patients admitted because of impending myocardial infarction. Am Heart J. 1982;103(4 Pt 2):730-736.
- Rhinehardt J, Brady WJ, Perron AD, Mattu A. Electrocardiographic manifestations of Wellens’ syndrome. Am J Emerg Med. 2002 Nov;20(7):638-43. DOI: 10.1053/ajem.2002.35700.
- Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimský P; ESC Scientific Document Group. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119-177. doi: 10.1093/eurheartj/ehx393.
- Smith SW, et al. Diagnosis of ST-Elevation Myocardial Infarction in the Presence of Left Bundle Branch Block with the ST-Elevation to S-Wave Ratio in a Modified Sgarbossa Rule. Ann Emerg Med. 2012;60(6):766-776.
- Sgarbossa EB, Pinski SL, Barbagelata A, Underwood DA, Gates KB, Topol EJ, Califf RM. Electrocardiographic diagnosis of evolving acute myocardial infarction in the presence of left bundle-branch block. N Engl J Med. 1996 Feb 22;334(8):481-7. DOI: 10.1056/NEJM199602223340801
- Wagner GS, Macfarlane P, Wellens H, Josephson M, Gorgels A, Mirvis DM, Pahlm O, Surawicz B, Kligfield P, Childers R, Gettes LS, Bailey JJ, Deal BJ, Gorgels A, Hancock EW, Kors JA, Mason JW, Okin P, Rautaharju PM, van Herpen G. AHA/ACCF/HRS Recommendations for the Standardization and Interpretation of the Electrocardiogram: Part VI: Acute Ischemia/Infarction: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society. J Am Coll Cardiol. 2009 Mar 17;53(11):1003-11. DOI: 10.1016/j.jacc.2008.12.016.
- O’Gara PT, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines. Circulation. 2013;127(4):e362-e425.
- Tamis-Holland JE, et al. Contemporary Diagnosis and Management of Patients With Myocardial Infarction in the Absence of Obstructive Coronary Artery Disease: A Scientific Statement From the American Heart Association. Circulation. 2019;139(18):e891-e908.
- Collet JP, Thiele H, Barbato E, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation. Eur Heart J. 2021;42(14):1289-1367.
- Littmann L., “South African flag sign: a teaching tool for easier ECG recognition of high lateral infarct”, Am J Emerg Med. 2016 Jan;34(1):107-9
- PM Cardio. Powerful Medical. Available from: https://www.powerfulmedical.com/pmcardio.