Overview:
This state-of-the-art review explores the evolution of heart attack classification, challenging the limitations of the standard-of-care STEMI/NSTEMI framework. It advocates for a shift toward diagnosing heart attacks based on the presence of acute vessel occlusion rather than relying solely on standard ECG criteria. By redefining how myocardial infarctions are identified and managed, this approach has the potential to reduce misdiagnoses, optimize triage, and refine treatment prioritization in emergency cardiology.
Published In: Journal of the American College of Cardiology (JACC) – JACC Advances
Presented Date: November 03, 2024
Introduction
A generation ago thrombolytic therapy led to a paradigm shift in myocardial infarction (MI), from Q-wave/non-Q-wave to ST-segment elevation MI (STEMI) vs non-STEMI. Using STE on the electrocardiogram (ECG) as a surrogate marker for acute coronary occlusion (ACO) allowed for rapid diagnosis and treatment. But the vast research catalyzed by the STEMI paradigm has revealed increasing anomalies: 25% of “non-STEMI” have ACO with delayed reperfusion and higher mortality.
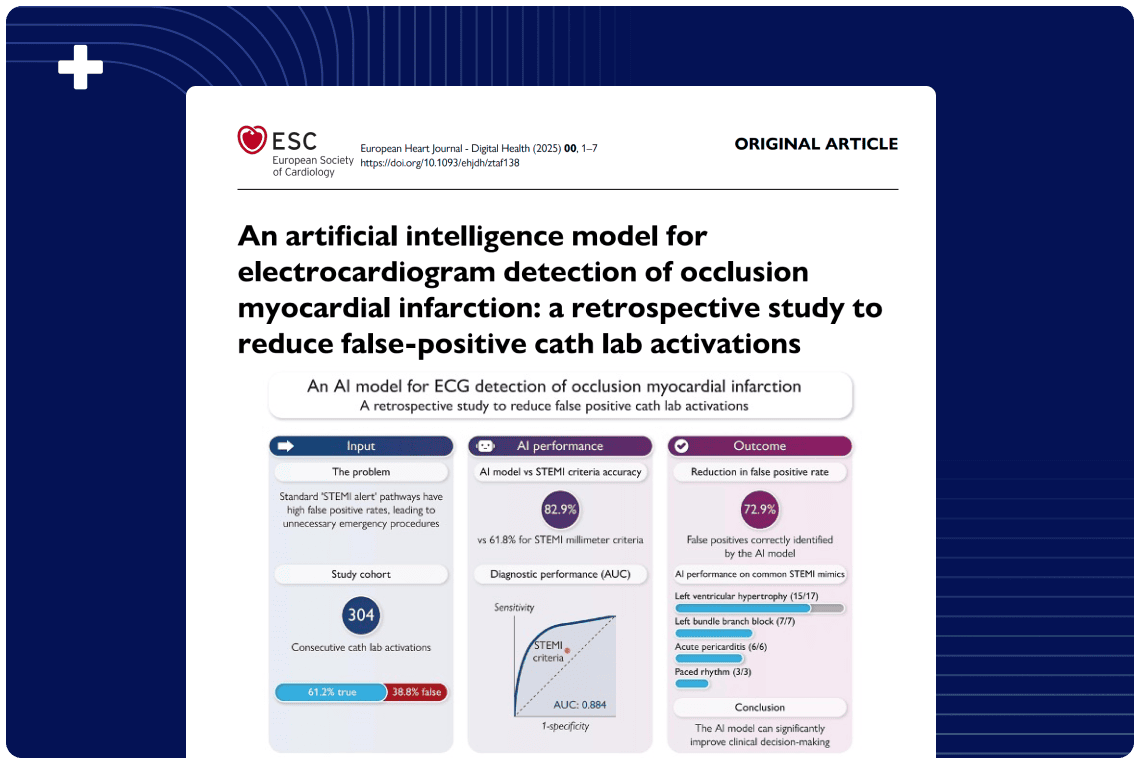
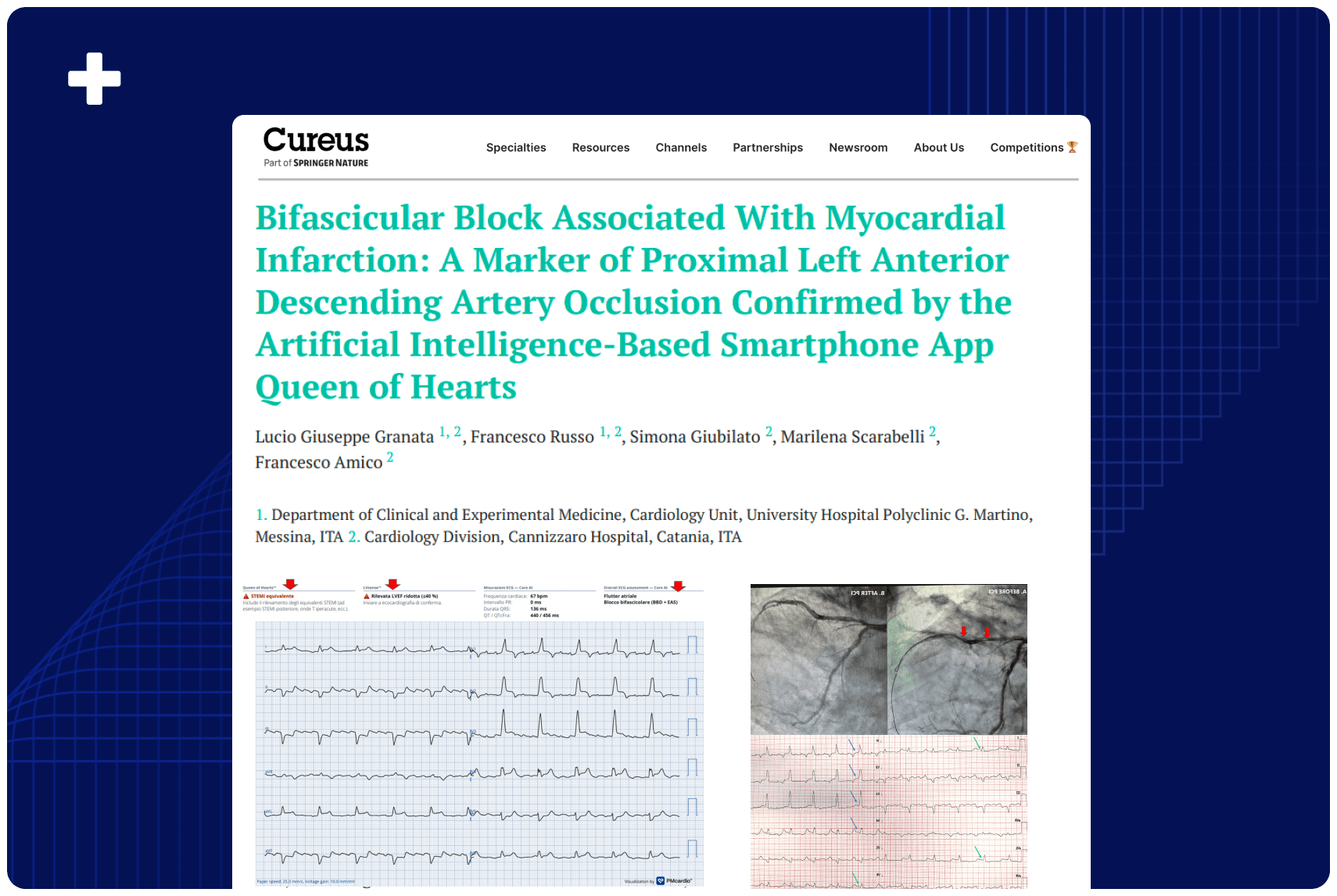
Studying these limitations has given rise to the occlusion MI (OMI) paradigm, based on the presence or absence of ACO in the patient rather than STE on ECG. The OMI paradigm shift harnesses advanced ECG interpretation aided by artificial intelligence, complementary bedside echocardiography and advanced imaging, and clinical signs of refractory ischemia, and offers the next opportunity to transform emergency cardiology and improve patient care. This State-of-the-Art Review examines the paradigm shifts from Q wave to STEMI to OMI.
Highlights
- The STEMI paradigm transformed emergency cardiology, but there is increasing recognition of its limitations.
- STEMI criteria is a poor surrogate marker for acute coronary occlusion, leading to delayed reperfusion.
- Evidence-based advances can identify OMI not meeting STEMI criteria, and false positive STEMI.
- The OMI paradigm harnesses advanced ECG interpretation aided by artificial intelligence, echocardiography, and advanced imaging.
Authors: Jesse McLaren, José Nunes de Alencar, Emre K. Aslanger, H Pendell Meyers, and Stephen W. Smith