Overview
This editorial proposes a shift in how we conceptualize acute coronary syndrome (ACS). The authors argue that the traditional STEMI vs. NSTEMI dichotomy is insufficient because it overlooks many cases of acute coronary occlusion that do not meet classic ST-elevation criteria. They introduce and advocate for an “Occlusion Myocardial Infarction (OMI)” paradigm—focusing on the pathophysiology of vessel occlusion rather than on a single ECG threshold—and call for broader adoption of more sensitive ECG interpretation tools, complementary imaging, and AI support to improve detection and outcomes in ACS.
Published in: Advances in Interventional Cardiology
Published on: 19 May 2025
Background
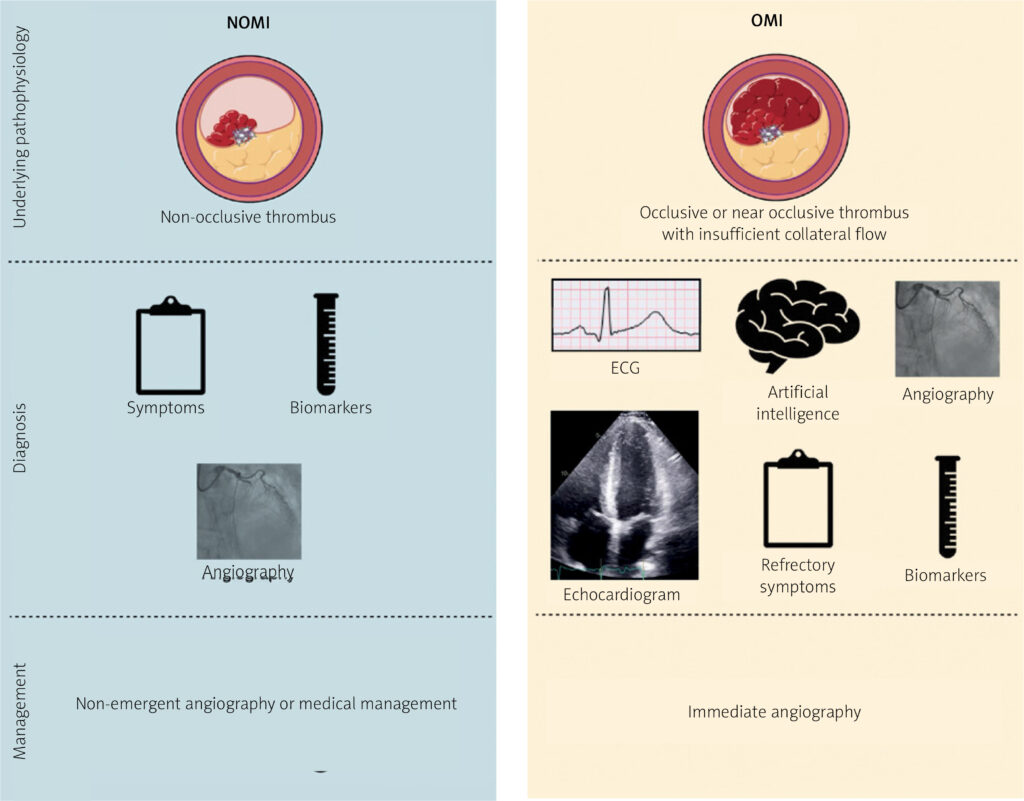
The STEMI/NSTEMI paradigm has long guided diagnosis and management: STEMI is assumed to correspond to a fully occluded artery and warrants emergent reperfusion, while NSTEMI is considered non-occlusive.
However, angiographic data over recent decades challenge this neat separation: a substantial fraction of patients classified as NSTEMI in fact have total occlusion of a culprit coronary vessel, and these patients have worse prognoses compared to non-occlusive NSTEMIs.
The authors note a “no false negative paradox” inherent in the classic paradigm, because patients without ST elevation but with occlusion are simply labeled NSTEMI, and false negatives are hidden in classification.
To remedy this, in 2018, the “OMI Manifesto” was proposed, promoting a paradigm based on the presence or absence of acute coronary occlusion (or near-occlusion with insufficient collateral flow), regardless of whether ST elevation is present.
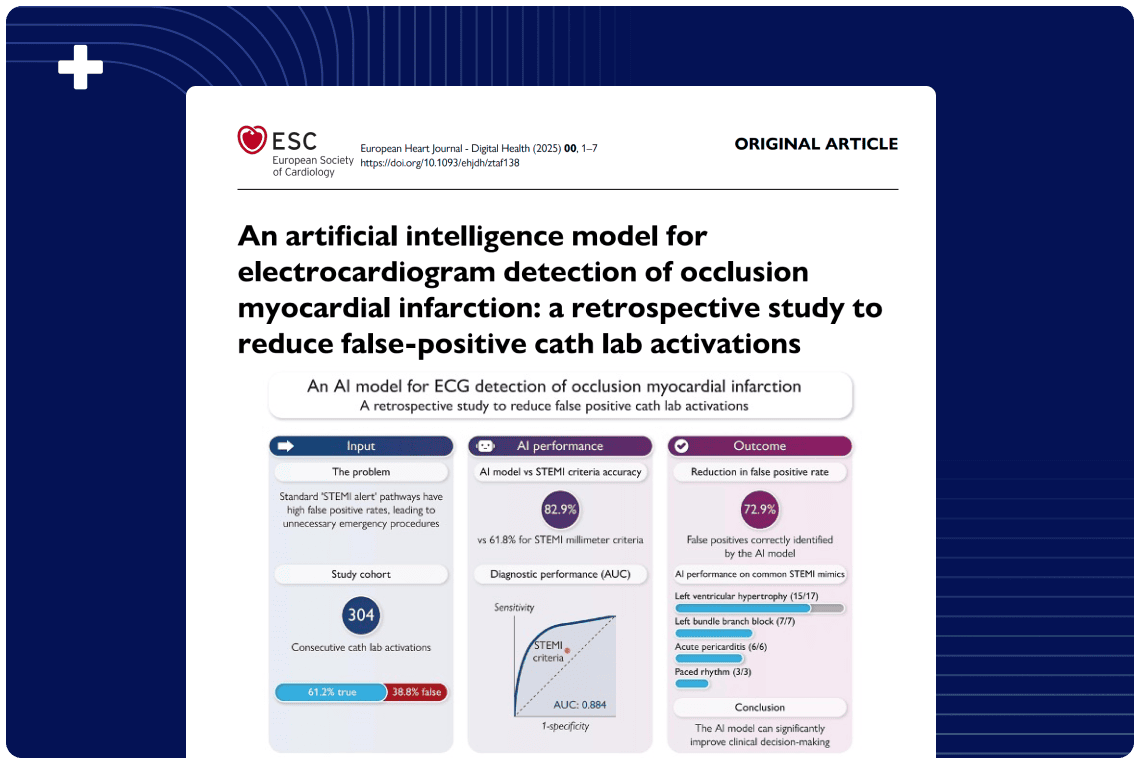
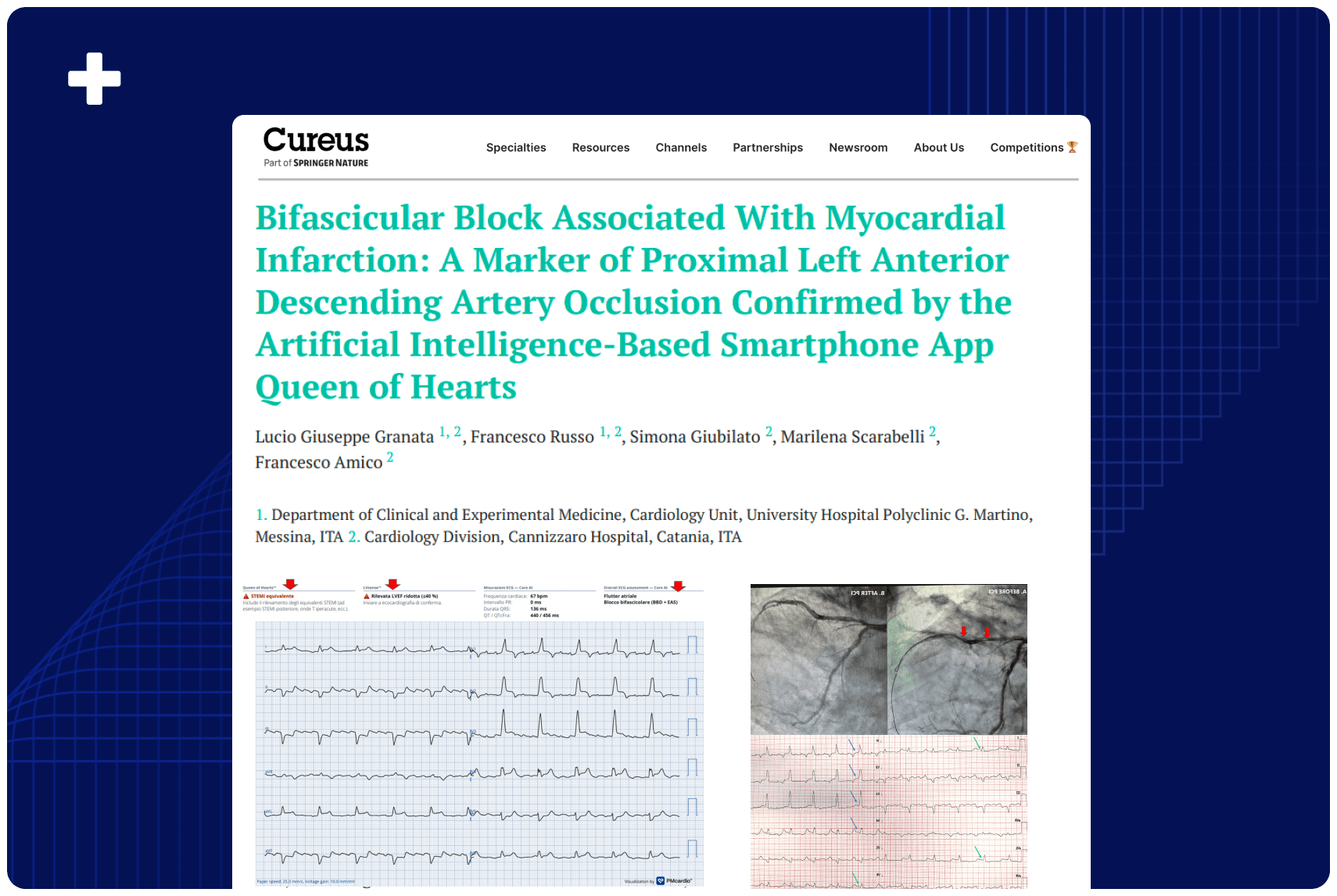
The authors assert that advances in ECG interpretation (including recognition of subtle signs like hyperacute T waves, ST depression in reciprocal leads, modifications in bundle branch block, etc.) and artificial intelligence make more sensitive detection of OMI feasible.
Methods
Because this is an editorial rather than an original research study, the “methods” are argumentative and literature-based rather than experimental. The authors:
Call for adoption of AI and systemic changes (e.g. registry definitions, quality metrics) to advance the OMI paradigm in real clinical care.
Review and synthesize existing angiographic and meta-analytic evidence on rates of coronary occlusion among patients without classic ST elevation.
Critique the limitations of the STEMI/NSTEMI paradigm and its entrenched influence on quality metrics and guideline approaches.
Present the concept of the OMI paradigm and survey supporting evidence, including studies where ECG reading under the OMI paradigm improved sensitivity without sacrificing specificity.
Illustrate specific ECG patterns that may portend occlusion despite the absence of ST elevation (e.g., hyperacute T waves, reciprocal changes, modified Sgarbossa criteria, etc.).
Results
Meta-analyses show that ~ 25–34 % of NSTEMI patients may harbor complete culprit artery occlusion, and that such patients have significantly worse outcomes than NSTEMI patients without occlusion.
Classic STEMI ECG criteria have limited sensitivity: pooled estimates suggest sensitivity as low as ~ 43.6 % for detecting acute coronary occlusion.
Advanced ECG interpretation under the OMI approach (including recognition of non-classic ECG patterns) has demonstrated improved sensitivity for detecting occlusion while maintaining specificity. For example, in prior studies, blinded readers using OMI criteria nearly doubled sensitivity for acute coronary occlusion compared to STEMI criteria.
The editorial also cites work showing that OMI vs. non-OMI classification better predicts mortality than STEMI vs. NSTEMI classification.
AI-based ECG models are emerging as promising tools to detect subtle ECG changes consistent with occlusion.
Conclusion
The authors conclude that the STEMI/NSTEMI paradigm is no longer sufficient and often misclassifies patients, thereby delaying or denying timely reperfusion to many true occlusions. The OMI concept reframes ACS classification around pathophysiology (occlusion) rather than rigid ECG thresholds. By applying refined ECG criteria, integrating AI, and changing guideline and quality metric frameworks, clinicians can better identify and treat patients at risk. The authors call for adoption of OMI in future ACS research, registries, clinical practice, and policy.