Overview
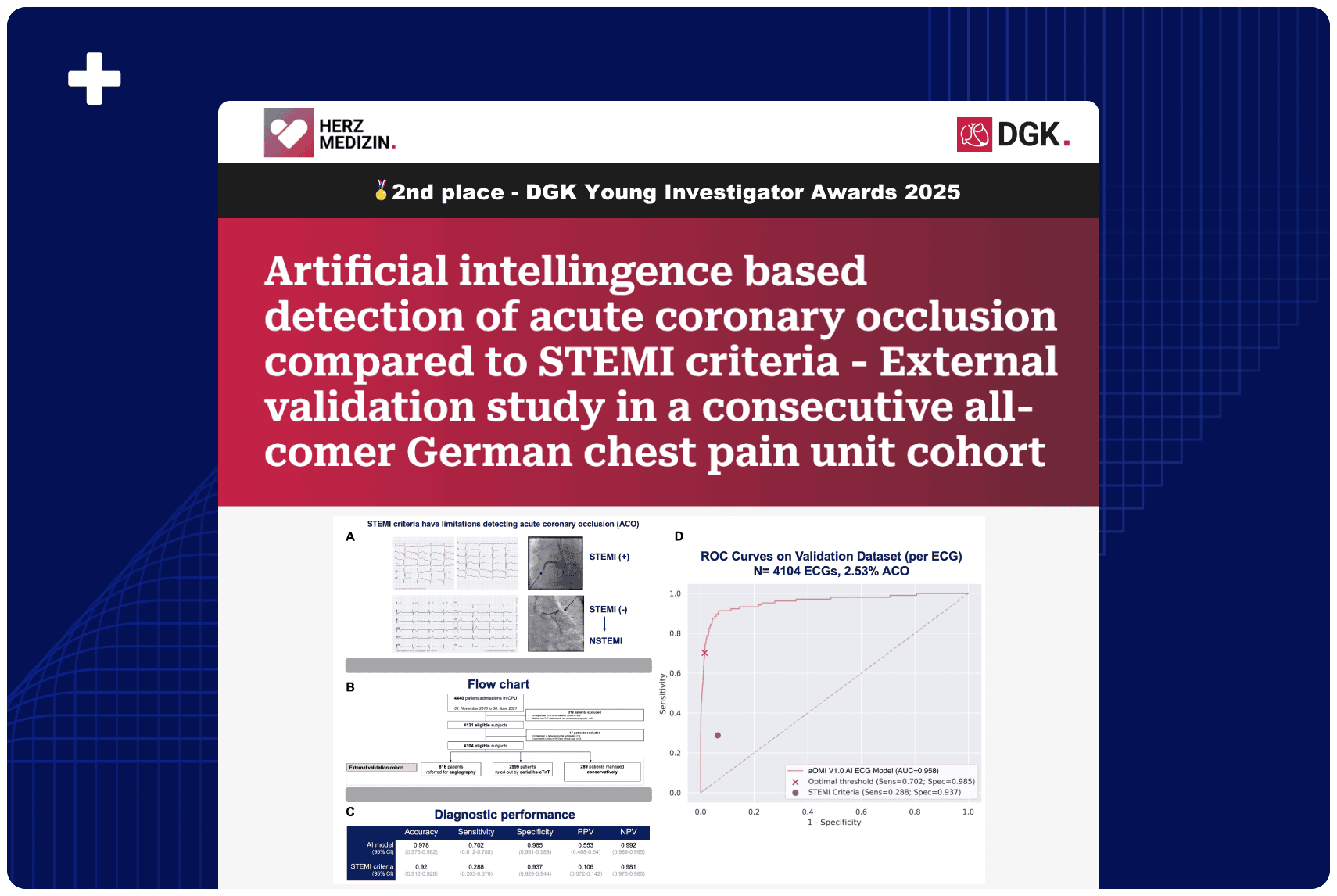
Conventional ECG criteria often fail to detect severe coronary blockages, leading to delayed treatment and worse outcomes. The team at Mt. Sinai Morningside performed a retrospective validation of the PMcardio STEMI AI ECG Model, demonstrating 81% sensitivity and 87% specificity in identifying high-risk patients. The AI model nearly doubled the sensitivity of STEMI criteria and correctly reclassified false positives, potentially reducing unnecessary catheterizations while ensuring no true heart attacks were missed.
Published In: Circulation (AHA Journals) – presented at the American Heart Association (AHA) 2024 Scientific Sessions
Presented Date: November 11, 2024
Background
Traditional ST-elevation criteria do not exhibit high sensitivity for acute occlusion detection, with many total occlusions presenting as NSTEMI, often resulting in worse outcomes. AI-based EKG interpretation may improve the identification of occlusion myocardial infarction (OMI). This study evaluates a novel AI-EKG device’s accuracy and clinical outcomes for detecting OMI in suspected ACS patients.
Methods
Adult patients who underwent coronary angiogram (CAG) at Mount Sinai Morningside Hospital for unstable angina, NSTEMI, or STEMI between January 1 and December 31, 2022, were included. The AI model (PMCardio) analyzed all pre-CAG ECGs. Inclusion criteria: suspected ACS at the emergency department, no outside hospital transfers, and available peak troponin levels. OMI was defined as a culprit vessel with TIMI 0-2 flow or TIMI 3 flow and peak cTnI > 10.0 ng/mL.
Primary outcome: AI EKG model’s sensitivity and specificity for predicting OMI on CAG. Secondary outcomes: F1 score, predictive values, AI OMI prediction of inpatient mortality, reduced ejection fraction at 1 year, unplanned readmissions, and STEMI criteria performance.
Results
Of 257 patients, 222 met the inclusion criteria: 72 STEMI (32%), 145 NSTEMI (65%), and 5 unstable angina (3%). Confirmed angiographic OMI: 60 (83%) STEMI and 51 (35%) NSTEMI patients. AI model sensitivity was 81.08%, specificity 87.39%, AUROC 0.8423, F1 score 0.8372, PPV 86.54%, NPV 82.20%. Odds ratio of 12.44 (1.56 – 98.98) for AI-detected OMI patients, unplanned readmissions (OR 1.15 [0.53 – 2.51]), and reduced ejection fraction at 1 year (OR 0.24 [0.26 -2 .16]).
Traditional STEMI criteria sensitivity for OMI was 54.05%, and specificity 89.29%. The AI model was 100% sensitive for STEMI-OMI and correctly reclassified 8 out of 12 false positive STEMI patients as NOMI.
Conclusion
The AI model nearly doubles the sensitivity of traditional STEMI criteria for OMI, enabling more accurate and earlier detection. Further studies are needed to determine if earlier OMI detection with AI improves clinical outcomes. The AI’s high specificity in detecting STEMI-OMI may also reduce false positive catheterization lab activations while ensuring no true positive STEMI OMI cases are missed.
Authors: James Choi, MBBS, Vincent Torelli, DO, Sara Diaz, MD, Esha Vaish, MBBS, Luka Katic, MD, Alex Nagourney, MD, Zara Khan, DO, Alex Silverman, MD, Serdar Farhan, MD