Overview
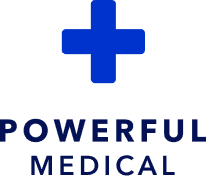
This single-centre retrospective study examined whether an AI-powered ECG model (PMcardio’s Queen of Hearts OMI model) can better detect acute occlusion myocardial infarction (OMI) and reduce false-positive cardiac catheterization laboratory (CCL) activations compared with traditional STEMI millimetre criteria. The authors analysed 304 consecutive STEMI pathway activations over a 2-year period at a tertiary academic centre and applied the AI model to pre-angiography 12-lead ECGs, comparing its performance against standard STEMI criteria. The AI model showed higher sensitivity (89.2% vs 68.3%), higher specificity (72.9% vs 51.7%), greater overall accuracy (82.9% vs 61.8%), and a high AUROC of 0.884 for identifying true OMI, while correctly flagging nearly three-quarters of false-positive activations as non-OMI. These findings suggest that integrating a specialized AI-ECG model into existing STEMI alert pathways could meaningfully reduce unnecessary CCL activations without compromising the detection of true occlusions.
Published in: European Heart Journal – Digital Health
Published on: 2 December 2025
Background
Current STEMI alert pathways largely rely on classic ST-segment elevation criteria to trigger emergent reperfusion, but their diagnostic performance is suboptimal. Up to 40% of frontline STEMI activations can be false positives, while a significant proportion of non-ST-elevation presentations still harbour an acutely occluded culprit artery, leading both to overuse of the CCL and to missed or delayed treatment of true OMI. Prior work has shown that STEMI criteria have limited sensitivity for OMI and that many NSTEMI patients have total occlusions that are not recognized by standard ECG rules. In parallel, deep neural network models trained on large ECG–angiography datasets have emerged as a promising alternative, capable of detecting STEMI and STEMI-equivalent patterns associated with angiographically proven acute coronary occlusions, and early implementation studies have hinted at reduced false-positive CCL activations and improved time to primary PCI. Against this backdrop, the present study set out to test, in an independent cohort, whether an AI-ECG OMI model could refine emergent CCL activation decisions within an existing “STEMI Alert” system.
Methods
The investigators conducted a retrospective analysis of consecutive adult patients for whom a STEMI alert and emergent CCL activation were triggered between January 2022 and December 2023 at a single tertiary academic medical centre. Eligible patients were at least 18 years old, had at least one standard 10-second 12-lead ECG available, and were managed via the standardized STEMI alert pathway. Exclusions included patients managed through other ACS protocols, urgent catheterizations for non-STEMI indications (such as high-risk PCI or mechanical support), death before catheterization, CCL activation solely for electrical instability (including cardiac arrest and ventricular storm without suspected STEMI), or absence of a usable ECG on which the activation decision was based.
Pre-coronary angiography ECG tracings were retrieved from the electronic medical record; when multiple ECGs were available, the one judged by chart review to have most influenced the activation decision was selected. True-positive OMI was defined by angiographic and biomarker criteria: an acute culprit lesion with TIMI 0–2 flow and any positive troponin, or TIMI 3 flow in combination with very high peak troponin thresholds. An interventional cardiologist, blinded to the AI outputs, adjudicated equivocal cases. All ECGs were digitized and analysed in batch mode by the CE-certified PMcardio platform using the Queen of Hearts AI ECG model (aOMI v1), which is a deep neural network trained to detect angiographically confirmed STEMI and STEMI-equivalent patterns irrespective of classic STEMI millimetre criteria. Test characteristics (sensitivity, specificity, accuracy, PPV, NPV, AUROC) of the AI model for OMI were calculated and compared directly with those of traditional STEMI millimetre criteria using standard paired statistical methods. The primary endpoint was the number of avoidable false-positive CCL activations, with diagnostic performance metrics as key secondary outcomes.
Results
Over the 2-year period, 454 CCL activations were screened; 148 were excluded based on predefined criteria or poor ECG quality, leaving 304 unique activations with analysable ECGs in the final cohort. The mean age was 60 ± 13 years and 76% of patients were male. Among these activations, 186 cases (61.2%) were adjudicated as true OMI and 118 (38.8%) as false positives. Of the false positives, the AI model correctly identified 86 cases (72.9% of false positives, 28.3% of the entire cohort) as not representing acute OMI, indicating a substantial potential reduction in unnecessary CCL activations if the AI output had been used prospectively. Conversely, among the 186 true-positive OMIs, the model correctly detected 166 cases (89.2%).
When formally compared with traditional STEMI millimetre criteria, the AI model demonstrated superior test characteristics for detecting true OMI. Sensitivity was 89.2% (95% CI 84.0–92.9) for the AI model versus 68.3% (95% CI 61.3–74.5) for STEMI criteria; specificity was 72.9% (95% CI 64.2–80.1) versus 51.7% (95% CI 42.8–60.5), and overall accuracy was 82.9% (95% CI 78.3–86.7) compared with 61.8% (95% CI 56.3–67.1). Positive and negative predictive values were also higher for the AI tool (PPV 83.8% vs 69.0%; NPV 81.1% vs 50.8%), and the AUROC for the AI model was 0.884 (95% CI 0.847–0.921), whereas a single fixed threshold STEMI criterion does not provide an AUROC. Subgroup and agreement analyses showed that in cases where the AI model and STEMI criteria disagreed, the AI prediction was substantially more likely to be correct, with disagreement favouring the AI tool in 82 of 100 discordant cases (odds ratio 4.6, 95% CI 2.7–8.1).
Conclusion
In this single-centre retrospective cohort, a dedicated AI-ECG model (PMcardio Queen of Hearts OMI) outperformed traditional STEMI millimetre criteria for detecting angiographically defined occlusion myocardial infarction among patients triggered through an existing STEMI alert pathway. The model combined high sensitivity with improved specificity, correctly identifying most true OMIs while flagging a large proportion of false-positive activations as non-OMI, thereby demonstrating clear potential to reduce avoidable CCL activations. These findings support the use of specialized AI-based ECG interpretation as a decision aid within STEMI systems of care, with the aim of refining activation decisions, improving resource utilization, and maintaining or enhancing timely treatment for patients with true acute coronary occlusion. Further multicentre and prospective studies will be important to confirm generalizability and to define how best to integrate such AI tools into real-world workflows.