Overview
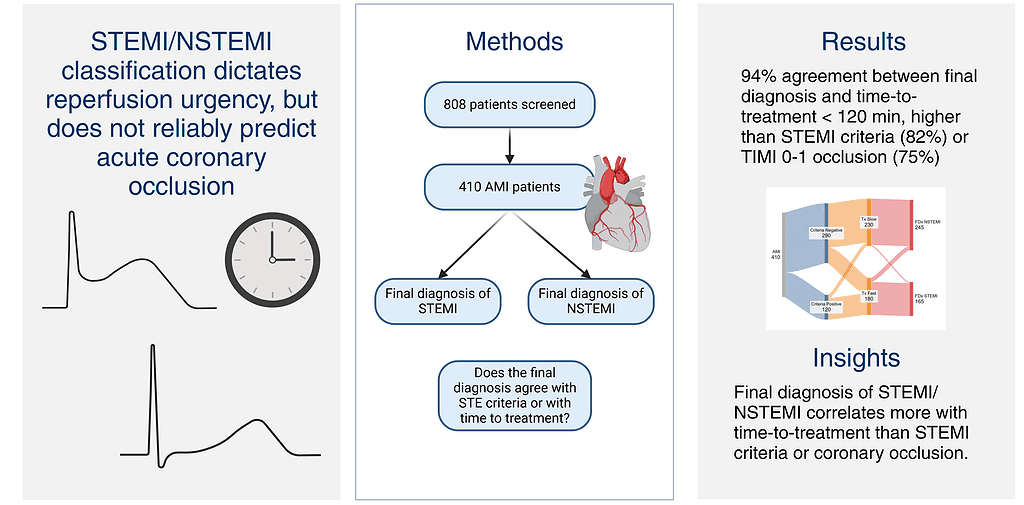
In a two-center registry study, investigators compared traditional STEMI/NSTEMI classification with angiographic and interventional diagnoses. Although guideline-defined ST-elevation criteria underpin quality metrics and reperfusion standards, they often fail to capture acute coronary occlusion myocardial infarction (OMI). This discordance has led to proposals for an OMI/Non-OMI paradigm, grounded in pathophysiology rather than ECG morphology. The study examined whether door-to-balloon time < 120 min aligns more closely with final cardiologist adjudication than either ST-segment elevation on ECG or angiographic evidence of TIMI 0–1 flow.
Published in: The Journal of Clinical Medicine
Published on: 18 September 2025
Background
The STEMI/NSTEMI paradigm underpins AMI management, yet often diverges from cath-lab practice. In a registry of 410 angiographically treated AMI patients, final diagnosis correlated most strongly with achieving door-to-balloon (D2B) < 120 min, showing 94% agreement, compared with 82% for ST-elevation and 75% for TIMI 0–1 flow. Discordance arose in 18% of cases, mainly when STE-negative patients were rapidly treated and labeled STEMI, or when STE-positive cases were delayed and labeled NSTEMI. Regression confirmed D2B as the sole predictor of discordance (OR 6.7). These findings suggest that quality-metric compliance, rather than electrocardiographic or angiographic criteria, exerts the greatest influence on the STEMI label.
Methods
This subanalysis of the DOMI-ARIGATO registry combined three prospectively captured cohorts of suspected ACS patients from two hospitals, including cath-lab activations, cardiology admissions, and ECG-based controls from UTROPIA. Patients were eligible if the interventional cardiologist (IC) explicitly documented a final diagnosis of STEMI or NSTEMI; late presenters were excluded. For each case, data extracted included final diagnosis (FDx), STEMI-criteria ECG status (STEc±), culprit lesion, TIMI flow, peak troponin, and time to angiography. STE was defined per the Fourth Universal Definition and adjudicated by two blinded reviewers. OMI was defined as a culprit lesion with TIMI 0–1 flow. Timely treatment was defined as angiography within 120 min of presentation, a pragmatic threshold encompassing both STEMI and high-risk NSTEMI guidelines. All cath reports were independently reviewed to confirm FDx. Statistical analyses included McNemar’s test for concordance and multivariable logistic regression for predictors of FDx/STE discordance, with collinearity checks and model calibration tests. A Sankey diagram was generated to visualize relationships among STE, treatment time, angiographic occlusion, and final diagnosis.
Results
Of 808 registry entries, 410 AMI patients with an explicit cath-lab diagnosis were analyzed: 165 STEMI and 245 NSTEMI. A door-to-balloon (D2B) time < 120 min showed the strongest concordance with final diagnosis (94%), compared with 82% for guideline ST-elevation and 74% for TIMI 0–1 flow. Diagnostic discordance occurred in 18% of cases, most often when STE-negative patients treated rapidly were labeled STEMI, or when STE-positive patients treated late were labeled NSTEMI. Multivariable analysis confirmed D2B < 120 min as the sole independent predictor of discordance (OR 6.7).
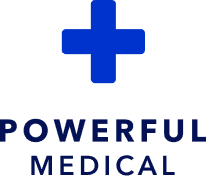
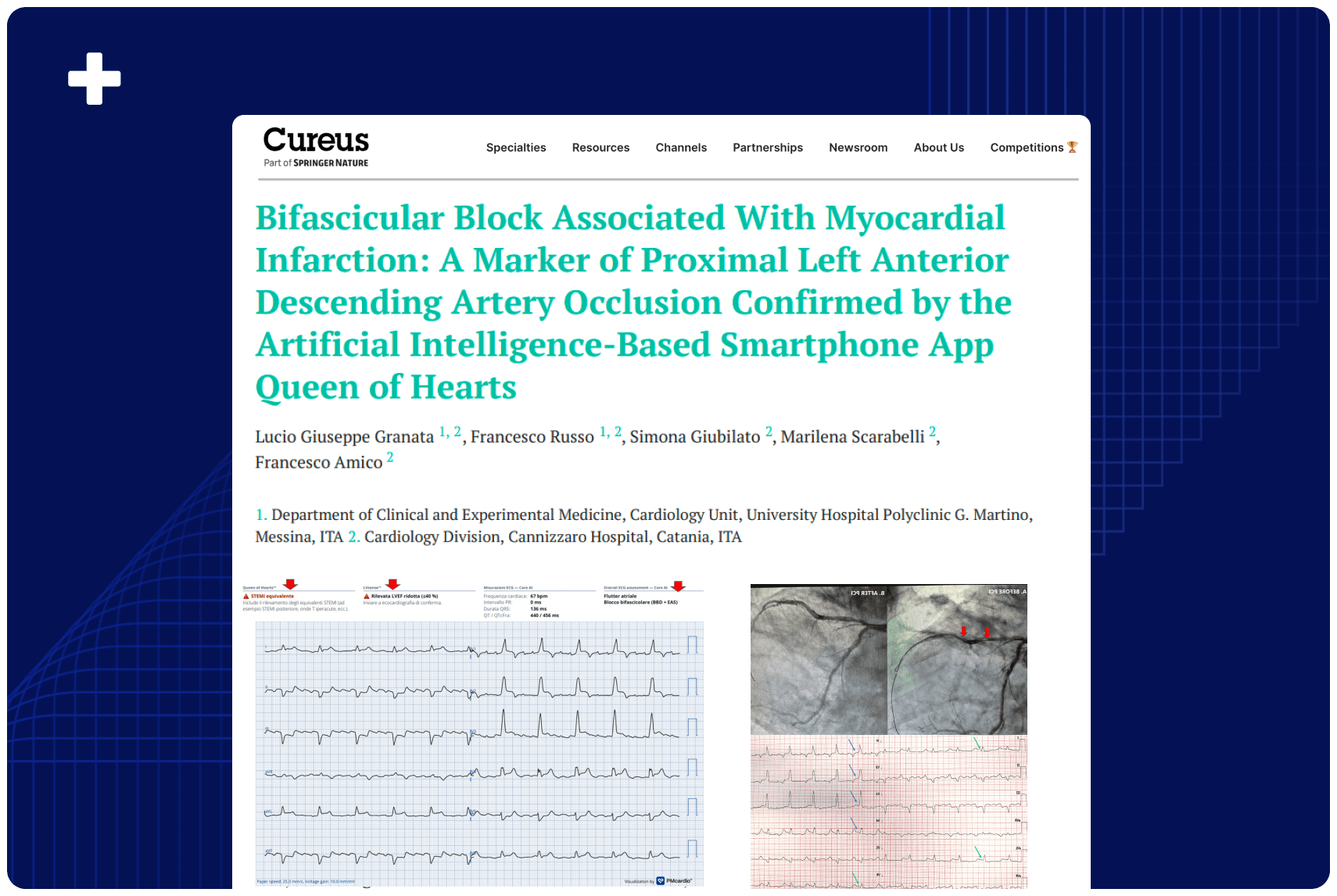
These findings indicate that the cath-lab “STEMI” label aligns more with treatment timelines than with ECG or angiographic evidence of occlusion. In practice, emergent reperfusion appears to dictate the diagnosis rather than the underlying pathology, raising concerns about the STEMI/NSTEMI paradigm as both a clinical tool and a quality metric. Subtle occlusions treated rapidly are often coded as STEMI, while delayed but ECG-positive occlusions fall under NSTEMI—masking missed opportunities for timely intervention. This systemic “time-drives-diagnosis” pattern underscores the need for pathophysiology-based frameworks such as the OMI model and for objective detection tools like AI-ECG to improve care and accountability.
Conclusion
In this retrospective analysis, time to treatment showed the strongest association. In the final diagnosis of STEMI vs. NSTEMI, more important than both the STEMI millimeter “criteria” and the presence or absence of total coronary occlusion. This has implications for research and quality improvement.
Authors: José Nunes de Alencar, Harvey Pendell Meyers, William Frick, Jesse T. T. McLaren, Stephen W. Smith