Overview
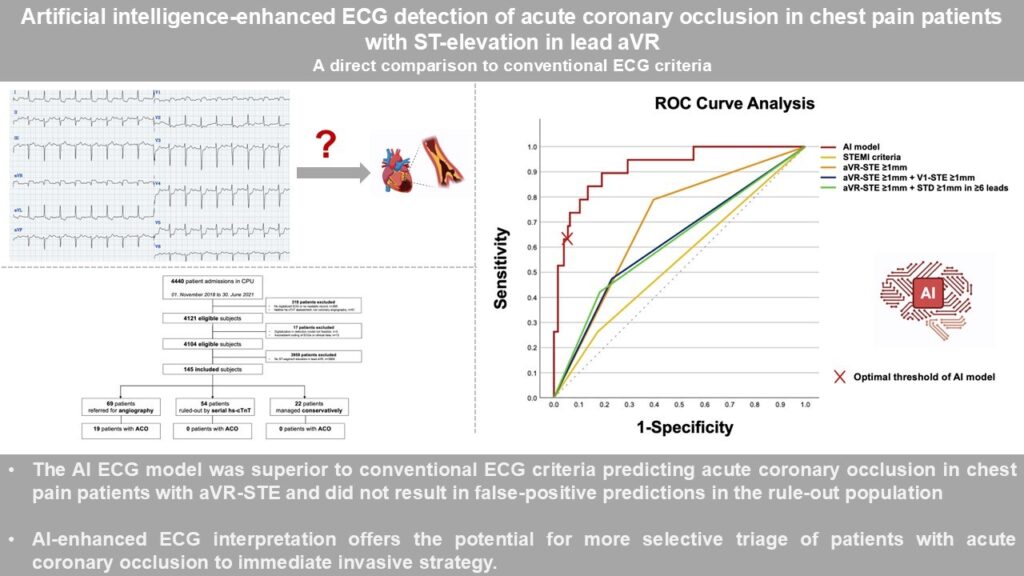
In a single‑centre retrospective study of 145 consecutive emergency‑department patients whose first ECG showed ≥1 mm ST‑elevation in lead aVR, investigators compared conventional electrocardiographic rules with a deep‑learning classifier (PMcardio “Queen of Hearts”) for recognising an acute coronary occlusion (ACO). Angiography and biomarker adjudication proved ACO in 19 patients (13 %). At an optimised probability threshold, the AI system achieved an area‑under‑the‑ROC curve of 0.918, detected 63 % of occlusions, and—crucially—generated no false‑positive calls in the 54‑patient rule‑out subgroup. By contrast, classic STEMI criteria identified only one in four occlusions and would have prompted between four and fourteen unnecessary emergency catheterisations.
Published in: European Heart Journal. Acute Cardiovascular Care
Published on: 09 July 2025
Background
ST‑elevation isolated to lead aVR, especially when accompanied by ST‑depression elsewhere, has long been viewed as an “occlusion pattern,” yet its prognostic and diagnostic value is undermined by frequent mimicry from diffuse subendocardial ischaemia and critical illness. Contemporary European Society of Cardiology guidance therefore equivocates, advising rapid angiography only when the clinical context appears high risk—a recommendation that inevitably trades sensitivity for an excess of potentially avoidable invasive procedures. The present analysis asked whether a convolutional‑network trained on occlusion‑MI (OMI) phenotypes could offer a more balanced triage strategy than any human‑devised threshold or pattern.
Methods
All adults presenting between November 2018 and June 2021 to the Cologne Chest‑Pain Unit with chest discomfort and ≥1 mm aVR ST‑elevation on the index ECG were enrolled. Printed or PDF tracings were digitised and processed by the PMcardio waveform converter before blinded inference by the AI model. Three common aVR algorithms (isolated aVR‑STE, aVR‑STE with V1‑STE ≥ 1 mm, and aVR‑STE with ≥1 mm ST‑depression in at least six leads) and fourth‑universal‑definition STEMI criteria were applied independently by two physicians. The reference diagnosis, “active ACO,” required a culprit lesion with TIMI 0‑1 flow plus biochemical or echocardiographic evidence of necrosis, and was adjudicated by an external cardiologist unaware of ECG findings. Diagnostic accuracy indices and receiver‑operating‑characteristic (ROC) curves were calculated for each rule.
Results
Of 4440 chest‑pain admissions screened, 145 met aVR‑STE entry criteria; 69 were taken directly to angiography, 54 entered serial high‑sensitivity troponin rule‑out, and 22 were managed conservatively. Nineteen patients (13.1 %) fulfilled the ACO definition. The AI model reached an AUC of 0.918, with 63 % sensitivity and 94 % specificity overall; within the troponin rule‑out arm it incurred no false positives. Conventional strategies were appreciably less balanced: STEMI criteria yielded an AUC of 0.644 and 26 % sensitivity, while the best of the bespoke aVR rules achieved 42 % sensitivity at only 42 % specificity. Had clinicians followed these rules in real time, four to fourteen additional patients without an occlusion would have undergone emergency angiography; adoption of the AI threshold would have averted every one of those procedures.
Conclusion
In the diagnostically challenging scenario of lead aVR ST‑elevation, traditional ECG heuristics combine inadequate sensitivity with a sizeable burden of false alarms. A single‑ECG deep‑learning model more than doubled case detection and virtually eliminated unwarranted catheter‑lab activations in low‑risk patients. These findings strengthen the case for a paradigm shift from millimetre‑based STEMI rules toward an occlusion‑centred framework in which expert or AI analysis guides prompt reperfusion.