Overview
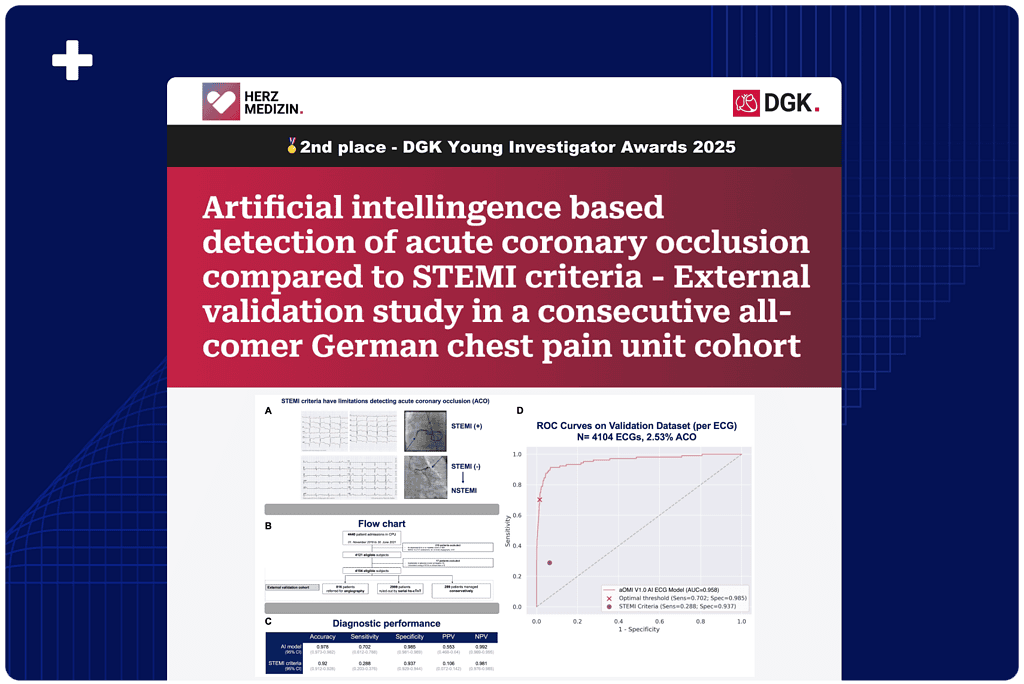
In a real-world cohort of over 4,000 chest pain patients presenting to a German CPU, excluding obvious STEMI heart attacks diagnosed before arrival, an AI ECG model detected serious artery blockages (ACO) with 97.8% accuracy. It outperformed traditional STEMI criteria, achieving higher sensitivity (70.2% vs 28.8%) and fewer false positives. This analysis earned second place at the 2025 DGK Young Investigator Awards in Germany.
Presented at: 91st Annual Meeting of the German Society of Cardiology (DGK)
Published Date: April 24, 2025
Background
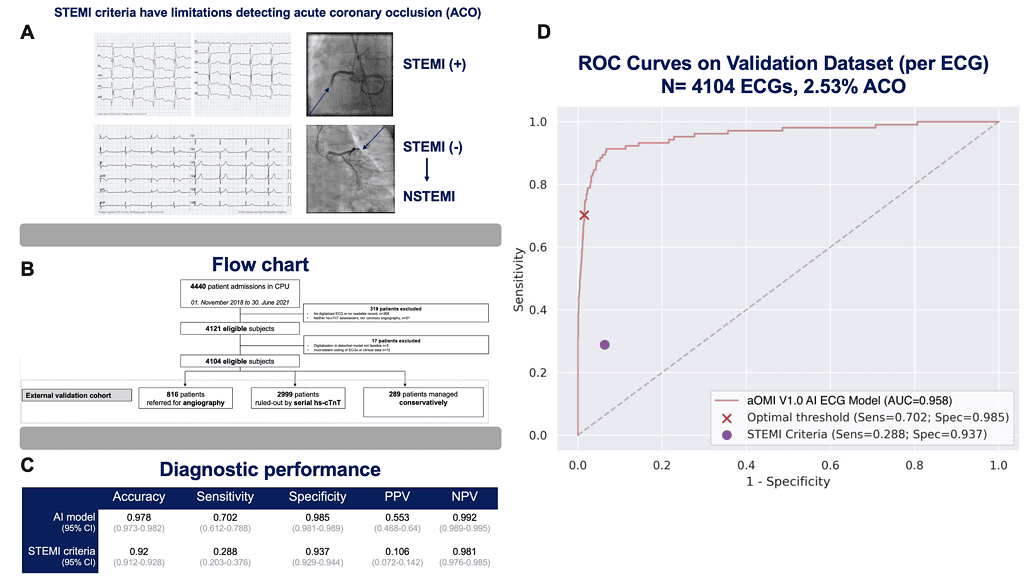
The 12-lead electrocardiogram (ECG) is essential to triage chest pain patients with suspected acute myocardial infarction (AMI). ST-elevation myocardial infarction (STEMI) criteria have a high specificity, but they lack sensitivity detecting acute coronary occlusion (ACO). On the one hand, 20-25% of AMI patients declared as non-STEMI have ACO (see A), these patients are at risk for delayed invasive management. On the other hand, STEMI criteria might be false positive resulting in overtreatment. Artificial intelligence (AI) based models offer the potential to improve the certainty of ECG based triage. Recent studies demonstrated promising results in detecting ACO in high-risk patient populations. Further evaluation of the utility in a broader chest pain unit (CPU) cohort is warranted.
We investigated the performance of an AI ECG model detecting ACO compared to STEMI criteria in an all-comer German metropolitan chest pain unit (CPU) cohort.
Methods
The AI model was derived from and validated in international cohorts including >12,000 chest pain patients. The present external validation cohort included all consecutive patients presenting with chest pain to a CPU in Cologne, Germany from 1st November 2018 to 30th June 2021. STEMI patients diagnosed in the prehospital setting bypassed the CPU and were excluded. Patient management and triage followed the contemporary ESC guideline including the high sensitivity cardiac troponin (hs-cTnT) algorithm (0/1h) whenever appropropriate. ACO was the primary outcome. ACO was adjudicated by an independent and blinded ECG expert (HPM) using biomarkers, angiographic outcomes and ECGs. The AI model’s diagnostic performance was assessed in the overall cohort and in the subgroup of ruled-out patients following 0/1h hs-cTnT algorithm. Receiver operating characteristic (ROC) analyses were performed.
Results
4440 patient admissions were registered in the CPU. Of these, 4104 were eligible for the present analysis (see B). The mean age was 54.5 (±19) years, 62.7% of patients were male. Overall, 19.9% of patients were referred for angiography while 73.1% were classified as low risk rule-out population following the hs-cTnT algorithm. The remaining patients (7%) were managed conservatively as they had elevated biomarkers, but were not referred for angiography. The prevalence of ACO 2.53% (n=104).
In ROC analysis the AI model had an area under the curve of 0.978 detecting ACO (see C). The model’s sensitivity was 70.2%, its specificity was 98.5%. This resulted in a negative predictive value of 99.2%. STEMI criteria reached an area under the curve of 0.92. The corresponding sensitivity was 28.8%, while the specificity was 93.7%. The negative predictive value of STEMI criteria was 98.1%.
In the subgroup of low risk patients ruled-out by hs-cTnT algorithm (n=2999) the AI model generated false positive results in 0.7% (n=20, specificity: 99.3%) of cases, compared to 5% (n=150, specificity: 95%) using STEMI criteria.
Conclusion
The AI ECG model demonstrated a remarkable diagnostic accuracy of 97.8% detecting ACO in an all-comer German CPU cohort. The AI model’s predictions outperformed conventional STEMI criteria: detection of ACO was more accurate and the AI model resulted in fewer false positive ACO diagnoses.
Future studies are required for prospective validation and to assess the use of AI based predictions compared to STEMI criteria or their equivalents in ad-hoc triage of chest pain patients.
Authors: Sascha Macherey-Meyer, H. P. Meyers, F. Hundehege, L. Krücken, S. Heyne, M. Meertens, K. Finke, V. Mauri, S. Baldus, S. Lee, C. Adler